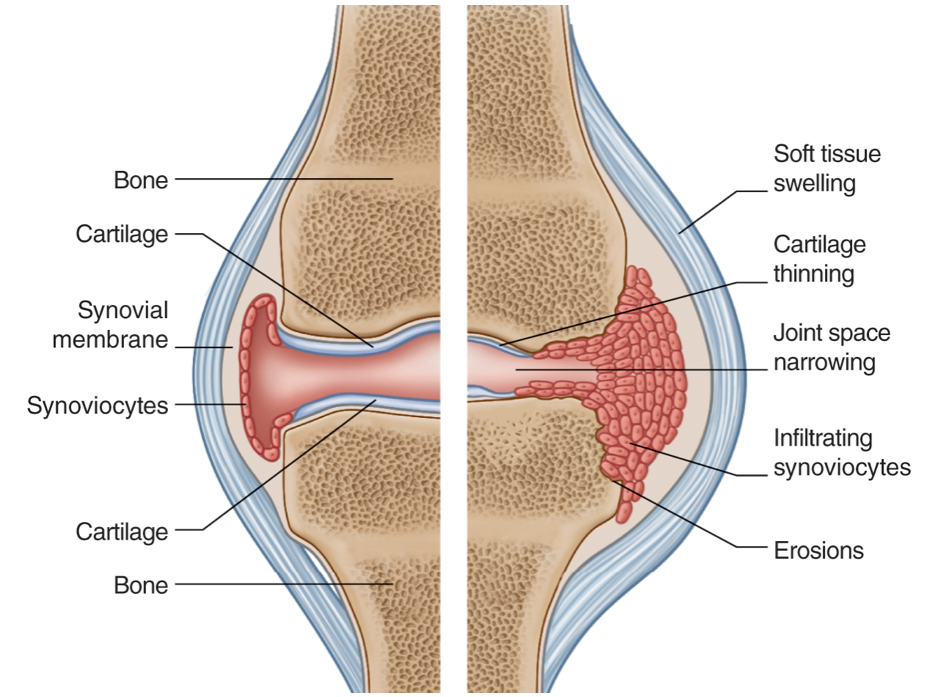
Joint Space
- In synovial joints, the congruent bony surfaces are lined with articular cartilage
- The joint space seen radiographically represents the two layers of radiolucent articular cartilage between the articulating bones
- Narrowing of this space is due to cartilage destruction
- Uniform/symmetrical narrowing may be across the joint space and is typical of an inflammatory arthritis.
- Concentric/asymmetric narrowing is typical of degenerative joint disease.
- In contrast joint space widening is secondary to occupation of and expansion of the joint space due to effusion (simple, inflammatory, infective/pus, hemorrhagic) and/or synovial proliferation.
Erosions
- An erosion is a non-traumatic defect of cortex or of the subchondral bone plate secondary to excessive local bone resorption and inadequate bone formation. Marginal/Periarticular In rheumatoid arthritis erosions are secondary to a combination of active synovial proliferation and high levels of inflammatory cytokines stimulating increased osteoclastic activity. An erosion is visible on radiographs as a defect in the cortex or subchondral bone plate
Erosion location
Can be helpful to decipher the underlying pathology e.g.Central
e.g. erosive OA, psoriatic arthritis.-
Central erosions may be a component of the “seagull” pattern characteristic of erosive osteoarthritis whereby central erosions occurs with marginal osteophytes and joint space loss.
 info_outline
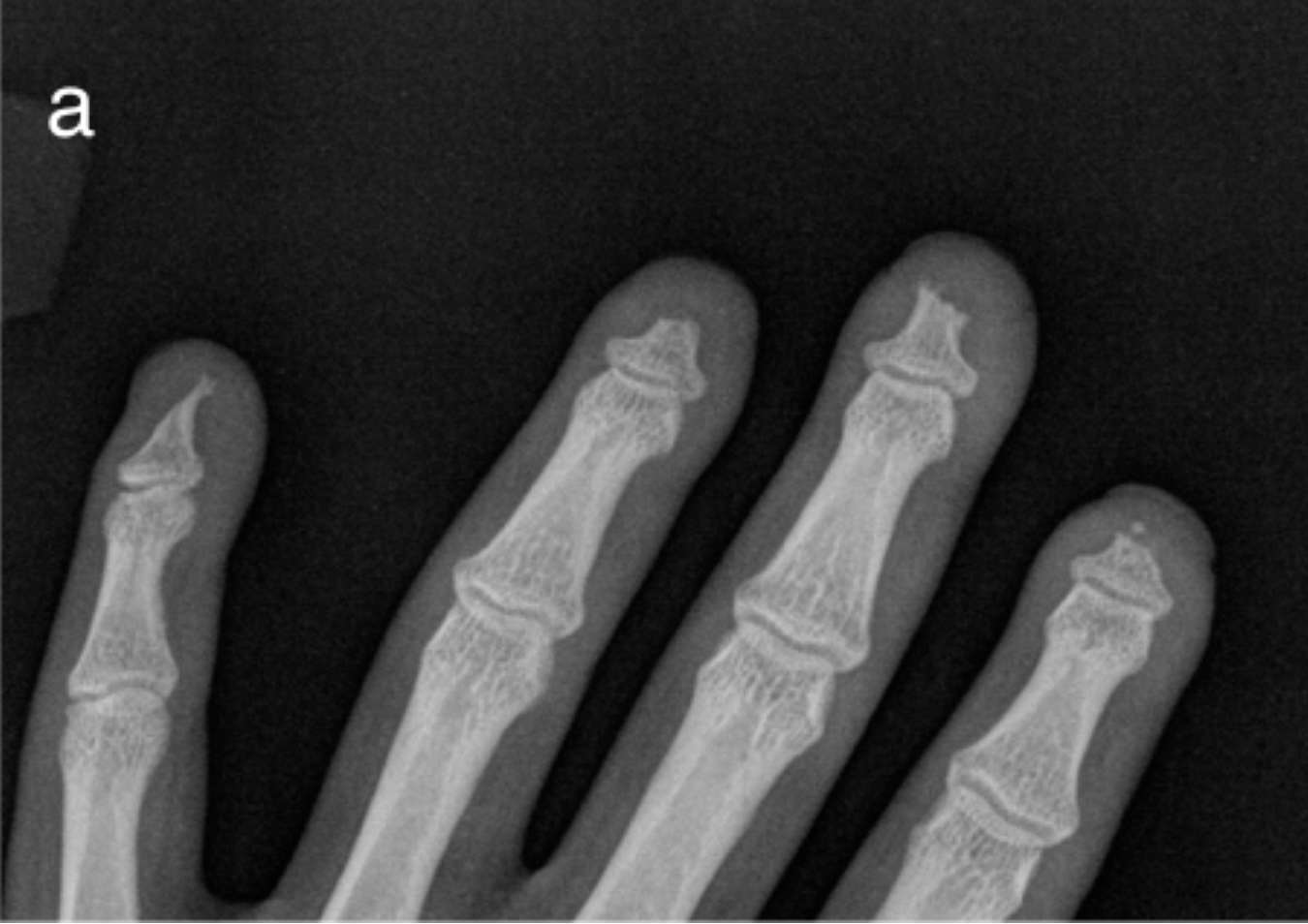
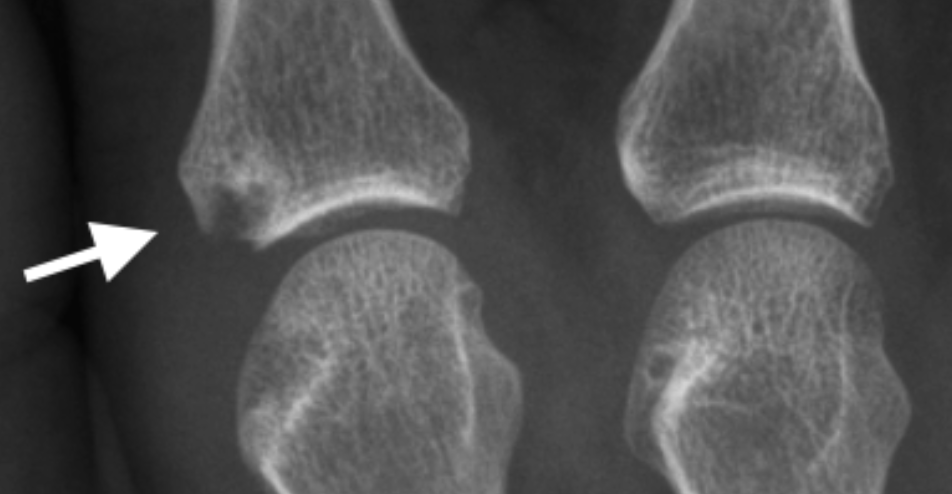
Central erosion (arrow) and osteophytes (arrowhead) at a PIPJ with a typical “Gull-wing” configuration in a patient with Erosive Osteoarthritis).
info_outline
Central erosion (arrow) and osteophytes (arrowhead) at a PIPJ with a typical “Gull-wing” configuration in a patient with Erosive Osteoarthritis). -
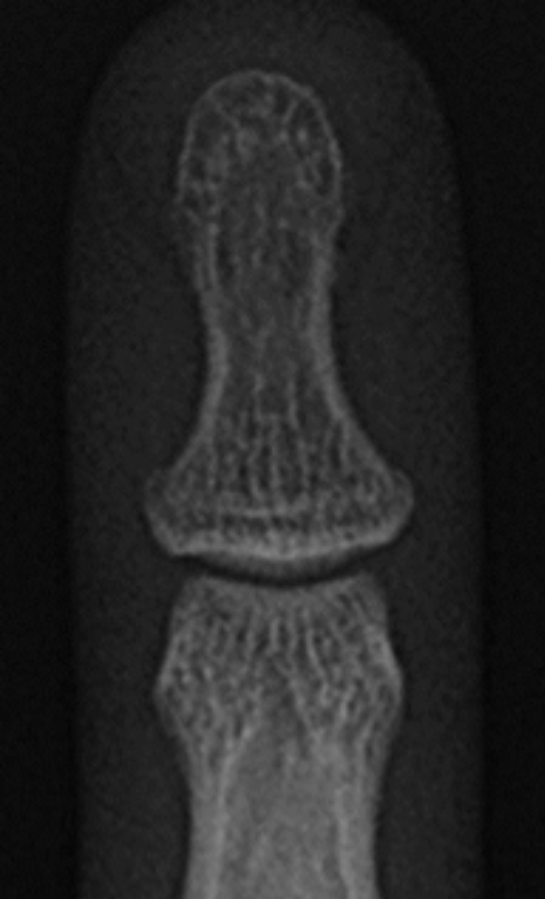
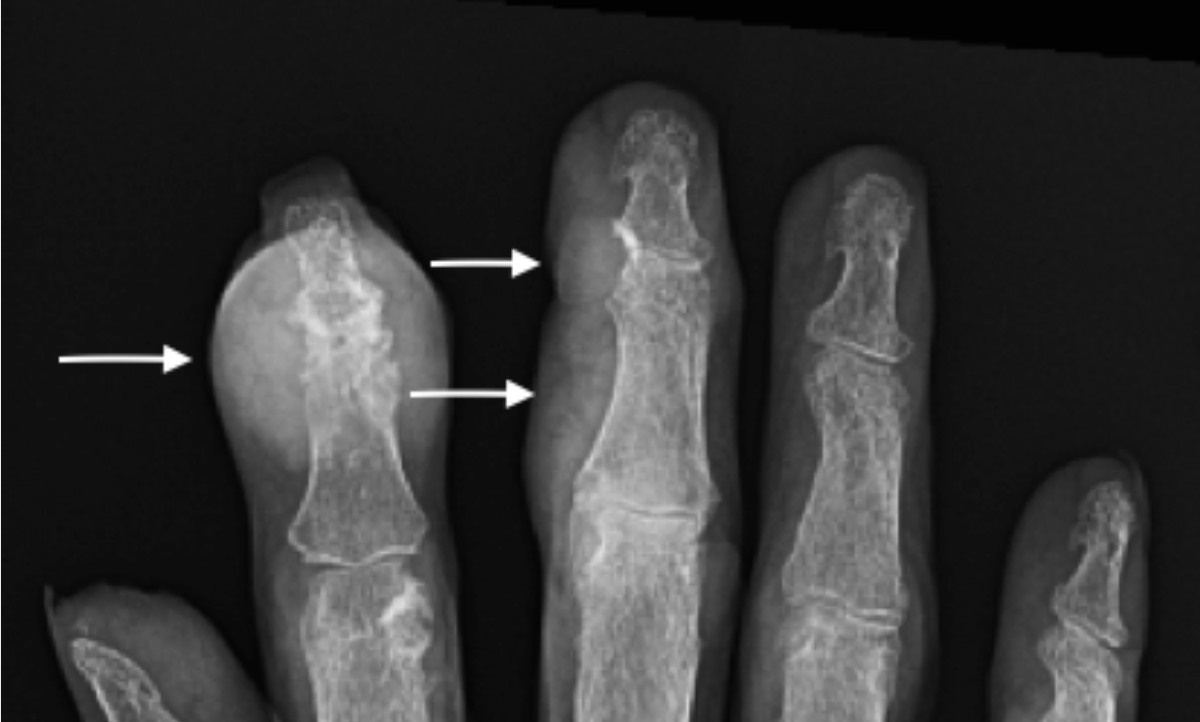
In psoriatic arthritis a “pencil-in-cup” erosion develops from a large central erosion on one side of the joint and marginal erosions with secondary whittling opposite side joint. The narrowed residual bone falls into the large erosion like a pencil in
a cup.
 info_outline
“Pencil-in-cup” erosion in a patient with longstanding Psoriatic Arthritis. Lateral radiograph demonstrates a large central erosion (arrow) of the distal phalanx and circumferential erosion head middle phalanx giving it a whittled appearance
info_outline
“Pencil-in-cup” erosion in a patient with longstanding Psoriatic Arthritis. Lateral radiograph demonstrates a large central erosion (arrow) of the distal phalanx and circumferential erosion head middle phalanx giving it a whittled appearance
-
Central erosions may be a component of the “seagull” pattern characteristic of erosive osteoarthritis whereby central erosions occurs with marginal osteophytes and joint space loss.
-
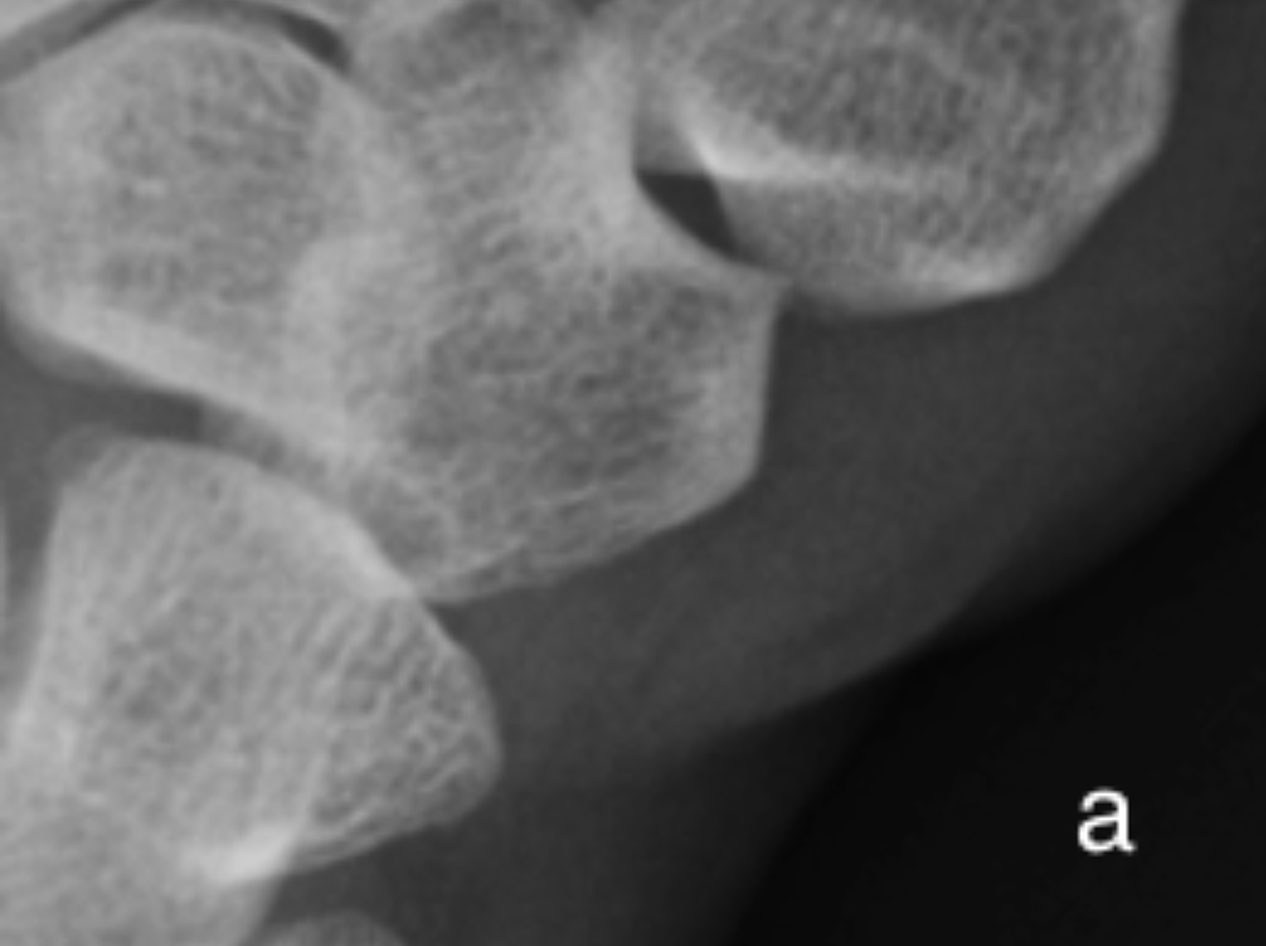
Marginal/periarticular
Marginal erosions can occur in the erosive spectrum of many arthropathies including rheumatoid arthritis, psoriatic arthritis, gout and septic arthritis. info_outline
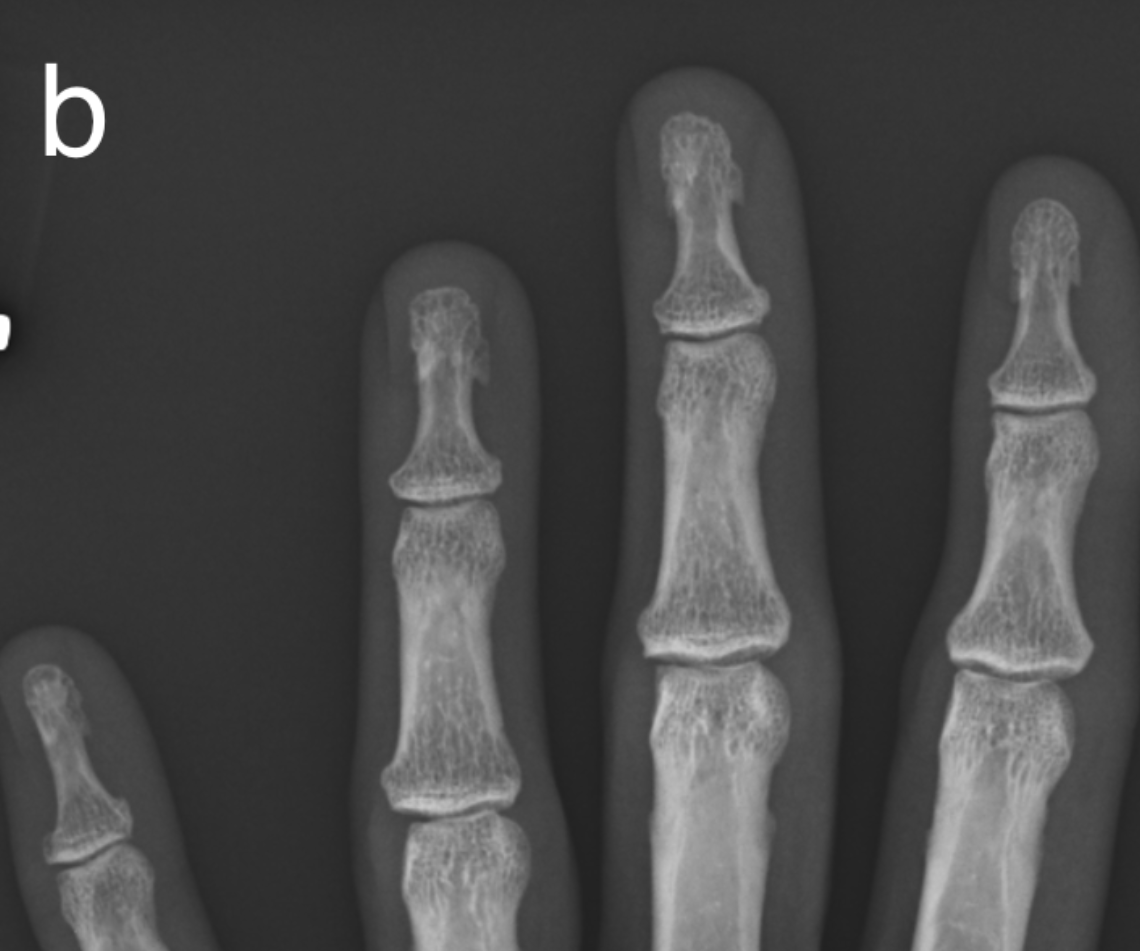
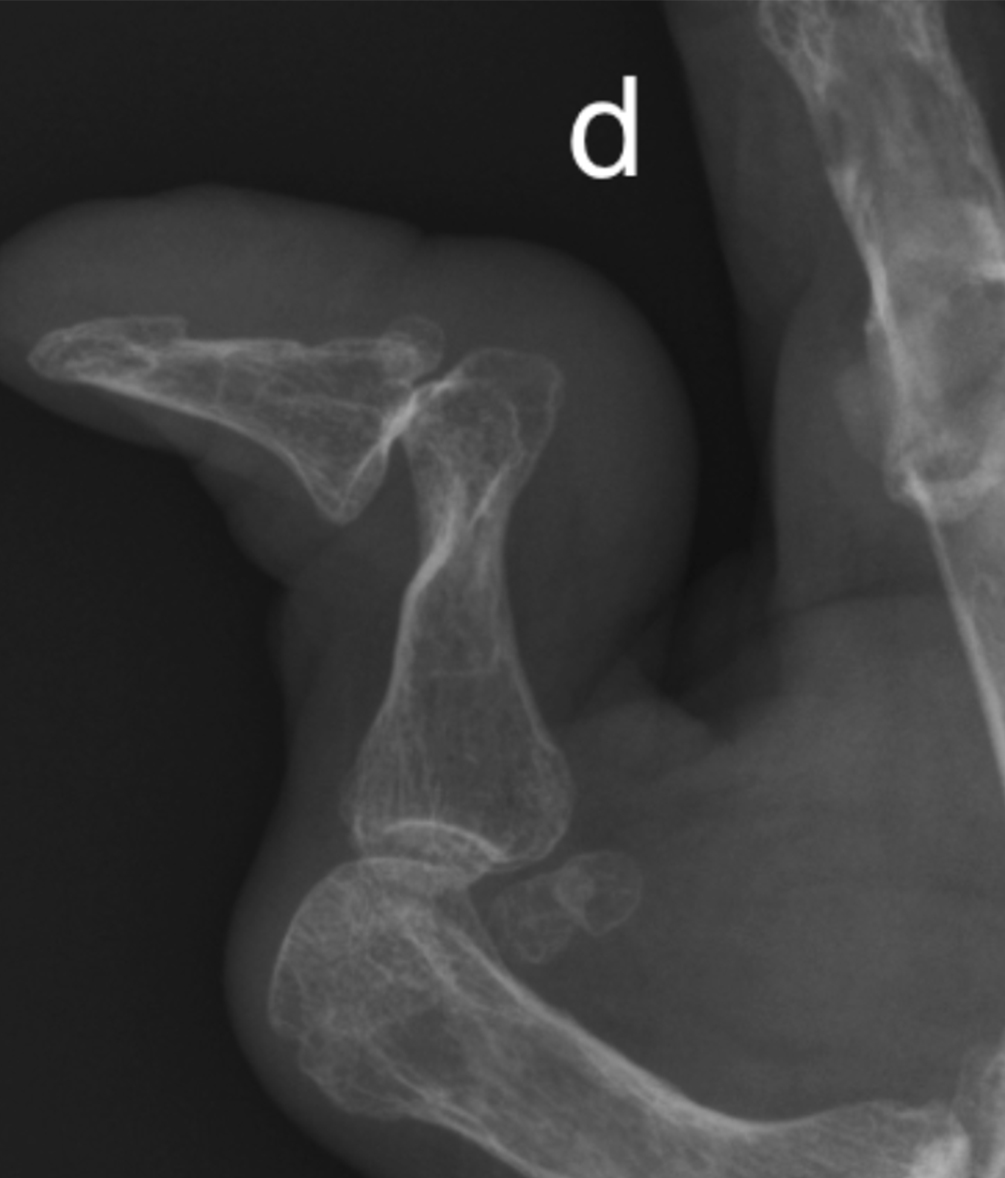
Marginal erosions in rheumatoid arthritis at a PIPJ. Most of the erosions have a lucent deep margin, lack a sclerotic border, in conjunction with mild periarticular osteopenia and soft tissue swelling suggest active disease.
info_outline
Marginal erosions in rheumatoid arthritis at a PIPJ. Most of the erosions have a lucent deep margin, lack a sclerotic border, in conjunction with mild periarticular osteopenia and soft tissue swelling suggest active disease. Juxta-articular
Or remote from the joint (gout).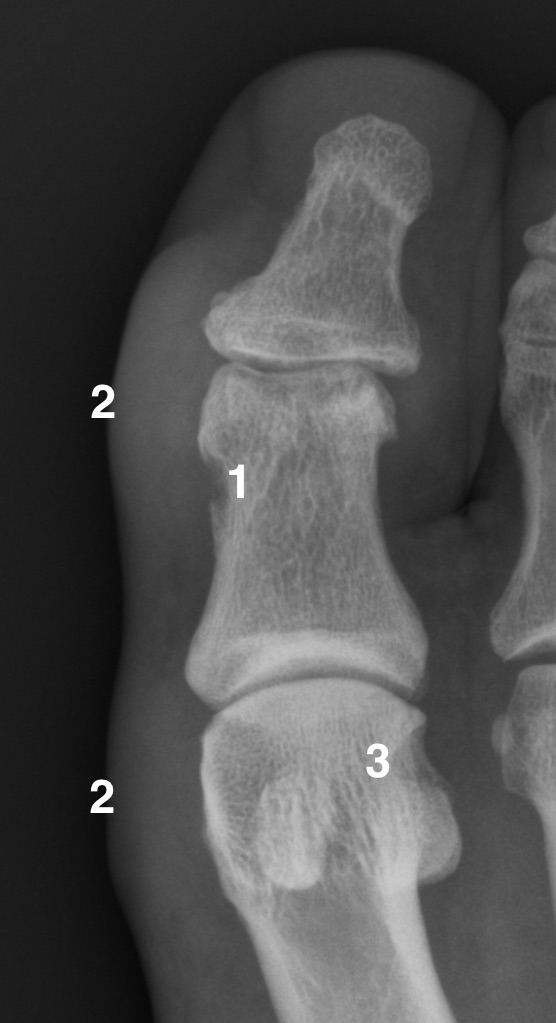 info_outline
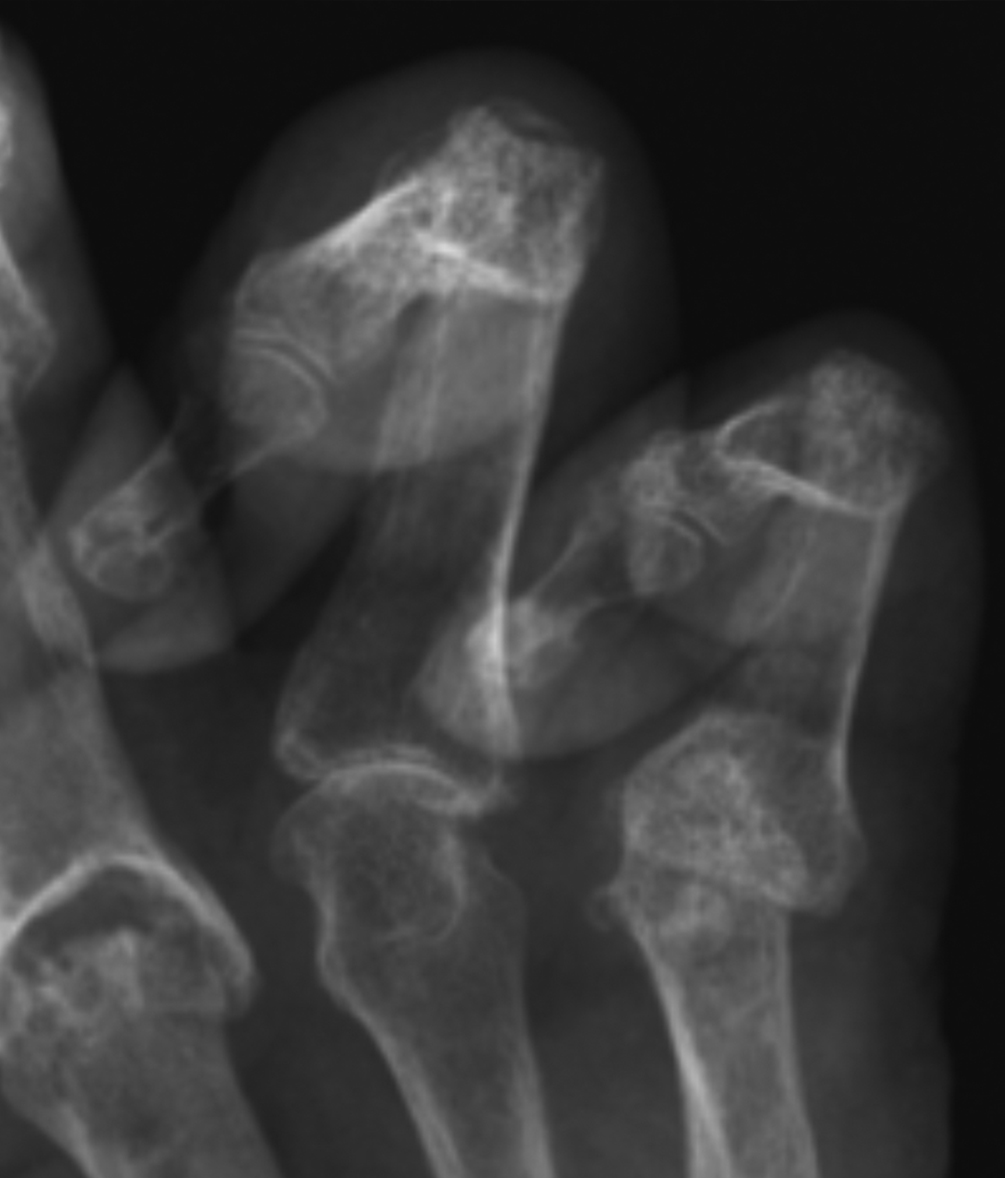
1 -Juxta-articular erosion 2-Tophus 3-Periaticular erosion
info_outline
1 -Juxta-articular erosion 2-Tophus 3-Periaticular erosion
Erosion margin
-
Sclerotic margin may indicate an inactive and healing erosion e.g. inactive rheumatoid arthritis. It can also be secondary to a pressure type erosion whereby the cortex is slowly eroded but mounts an osteoblastic response e.g. gout, PVNS.
 info_outline
Juxta-articular “punched-out” erosion (curved arrow), marginal erosion (arrow) and soft tissue tophus (line) in a patient with chronic gout. Note the maintained joint space, classically seen in gout ,and the sclerotic margins of the erosions.
info_outline
Juxta-articular “punched-out” erosion (curved arrow), marginal erosion (arrow) and soft tissue tophus (line) in a patient with chronic gout. Note the maintained joint space, classically seen in gout ,and the sclerotic margins of the erosions. - Erosions with a lucent margin indicate active disease
 info_outline
Subchondral sclerosis (arrows) demonstrated as ill-defined region of increased sclerosis (white on radiograph)
info_outline
Subchondral sclerosis (arrows) demonstrated as ill-defined region of increased sclerosis (white on radiograph)
-
Sclerotic margin may indicate an inactive and healing erosion e.g. inactive rheumatoid arthritis. It can also be secondary to a pressure type erosion whereby the cortex is slowly eroded but mounts an osteoblastic response e.g. gout, PVNS.
Subchondral Sclerosis
- The subchondral region is located deep to the subchondral bone plate which separates it from the articular cartilage.
- When this cartilage is damaged or lost as in osteoarthritis the subchondral bone is directly exposed to stresses across the joint with subsequent trabecular collapse and flattening, appearing ivory like with a polished surface termed eburnation and appearing as subchondral sclerosis on x-ray.
- Subchondral sclerosis is a region of increased bone density and thus appears on radiographs as an ill-defined region of dense bone (white) with a graduated return to normal bone density as one extends away from the joint
 info_outline
info_outline
(a) A normal 1st metacarpal CMC is shown for comparison
 info_outline
info_outline
(b) Subchondral sclerosis, eburnation, on both sides of the 1st CMC in this patient with osteoarthritis. Note joint space loss and intra-articular loose ossified bodies (avulsed osteophytes)
 info_outline
info_outline
Subchondral sclerosis (arrows) demonstrated as ill-defined region of increased sclerosis (white on radiograph)
Subchondral Cyst
- Subchondral cysts develop between the deformed trabeculae in areas of eburnation. Cysts are variable in size and have a thin sclerotic margin.
- Cysts may communicate with the joint in which case there is a defect in the overlying cortex/subchondral bone plate. This defect may be invisible radiographically or it may be large and simulate an erosion.
- Large subchondral cysts raise the possibility of underlying crystal disease.
- Subchondral cysts are also known as geodes.
Example Radiograph
 info_outline
info_outline
a) Subchondral cyst (arrow) base first metacarpal at the 1st CMCJ in a patient with osteoarthritis. Note that the subchondral bone plate is intact (curved arrow). There is also joint space loss, subchondral sclerosis and radial subluxation of the first
 info_outline
info_outline
b) Normal radiograph for comparison
Osteophyte
- In a degenerative joint, in regions of lower stress there is increased vascularisation in the subchondral regions which in turn stimulates endochondral ossification and subsequent osteophyte formation.
- Radiographically this appears as new bone formation growing laterally as an extension of the joint margin in a degenerative joint.
Example Radiograph
 info_outline
info_outline
Fused second PIPJ (arrow) in psoriatic arthritis
 info_outline
info_outline
2nd and 3rd MCPJ osteophytes (arrows)
Ankylosis
- Ankylosis refers to abnormal rigidity of a joint. It commonly refers to bony ankylosis whereby new bone formation bridges the joint space and eventually the two opposing bones become fused.
- Ankylosis may be partial or complete.
- It can be graded by the % of the joint that is ankylosed.
- It is a non-specific finding and may be congenital, post-traumatic, post-surgical but also seen in arthropathies including seronegative spondyloarthropathies, erosive osteoarthritis and longstanding rheumatoid arthritis
Example Images
 info_outline
info_outline
a) Longstanding rheumatoid arthritis with diffuse carpal fusion. Note osteopenia and extensive radial erosions.
 info_outline
info_outline
b) Normal radiograph for comparison
Acro-osteolysis
- Acro-osteolysis is osteolysis or erosion involving the terminal tufts of the phalanges
- It is associated with numerous disease processes including many rheumatological conditions such as hyperparathyroidism, psoriatic arthritis, scleroderma, Raynaud’s disease, dermatomyositis and juvenile idiopathic arthritis.
Example Radiograph
 info_outline
info_outline
a) Acro-osteolysis/resorption of the distal tufts in a patient with scleroderma
 info_outline
info_outline
b) normal radiograph for comparison
Osteopenia
- Decreased bone density or demineralization
- Appears radiographically as a decreased density of bone i.e increased lucency.
- In inflammatory arthritis periarticular osteopenia is a common finding in active disease e.g. rheumatoid arthritis (RhA), septic arthritis.
- In RhA it is related to high levels of inflammatory cytokines including tumor necrosis factor (TNF)-alpha and interleukin (IL)-6 and IL-17.
- In gout and seronegative spondyloarthropathies periarticular osteopenia is classically absent.
Example Radiograph
 info_outline
info_outline
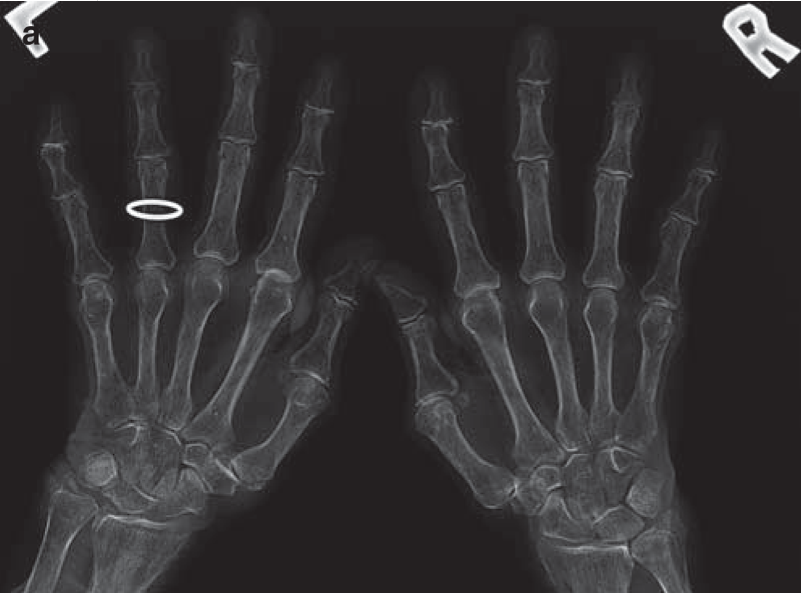
a) Significant periarticular osteopenia at the MCPJs in a patient with early active Rheumatoid arthritis
 info_outline
info_outline
b) normal radiograph for comparison
Osteoporosis
- Osteoporosis is a systemic disorder of bone metabolism characterized by a decreased bone mineral density and deterioration in bone microarchitecture.
- There is a decline in both bone quality and quantity
- Hand radiographs in osteoporotic patients may reveal characteristic findings. There is diffuse increase in lucency with thinning of cortex and trabeculae.
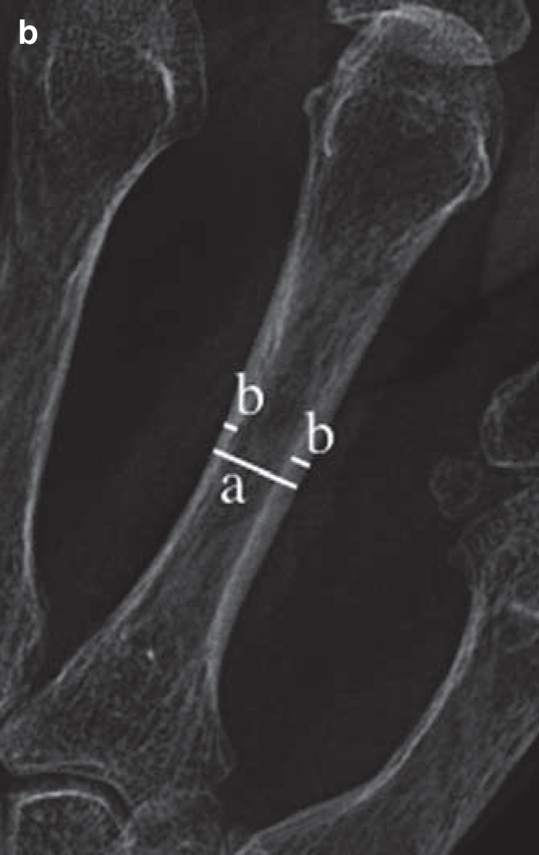
- The metacarpal index is a useful tool in the assessment of osteoporosis and has been shown to be associated with risk of hip fracture.
Metacarpal index:
 info_outline
info_outline
a) PA radiographs of the hands demonstrating osteoporosis
 info_outline
info_outline
b) calculation of the metacarpal index of the non-dominant second metacarpal at the mid-diaphysis. Measure the width bone {a} and the combined cortical thickness {b}, Metacarpal Index = b/a. References are available for different age groups and ethnicity.
In general normal values are greater than 50%.
Subperiosteal Resorption
- Osteoclastic activity is increased in response to increased PTH levels.
- Subperiosteal Resorption refers to osteoclastic bone resorption on the periosteal surface
- This is a specific finding in hyperparathyroidism.
- Classically affects the radial aspect of the proximal and middle phalanges of the 2nd and 3rd digits.
- Check radiograph for acro-osteolysis (tuft resorption), Brown tumors and chondrocalcinosis which may also be present in hyperparathyroidism.
Example Radiograph
 info_outline
info_outline
a) Subperiosteal Resorption along the radial aspects of the 2nd and 3rd digits (Hyperparathyroidism). Note also marginal erosion at the third DIPJ.
 info_outline
info_outline
b) Normal radiograph for comparison
Periostitis
- Periostitis refers to formation of periosteal new bone as a result of inflammation of the periosteum.
- It occurs in response to injury or other insult to cortical bone including trauma, tumors, metabolic diseases and some arthritides
- In arthritis, periostitis is most commonly seen in psoriatic and reactive arthritis
Example Radiograph
 info_outline
info_outline
PsA with diffuse soft tissue swelling (dactylitis) 4th digit and periosteal new bone formation proximal and middle phalanges (arrows).
Enthesophyte
- An Enthesophyte is abnormal new bone formation at the insertion of ligament, tendon or capsular attachment to bone (enthesis) in response to stress or inflammation at that site.
- Common sites include the iliac crests, patella (quadriceps and patellar tendons) and calcaneus (Achilles tendon).
- Uncommon in the hand radiograph, usually seen in seronegative arthritis at capsular attachment sites, e.g.PsA
Example Radiograph
 info_outline
info_outline
Enthesophyte formation (arrow) at capsular attachment DIPJ in a patient with PsA. Note new bone formation (line) more distally that is commonly seen in PsA.
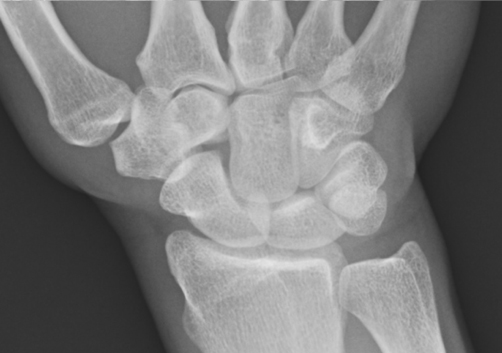
Chondrocalcinosis
- Chondrocalcinosis refers to calcification of cartilage, hyaline or fibrocartilage
- Involvement of hyaline cartilage causes increased density of the cartilage which then become visible on radiographs. Not commonly seen on hand radiographs but can be seen in larger joints such as the knee.
- Calcification of fibrocartilage, triangular fibrocartilage at the wrist, appears as linear increased attenuation of the TFC, separating the distal radioulnar and radiocarpal joints.
- Ligamentous calcification, commonly the scapholunate and lunotriquetral, is often present.
- It is usually, but not always, due to calcium pyrophosphate deposition.
Example Radiographs
 info_outline
info_outline
a) Chondrocalcinosis of the triangular fibrocartilage (arrow) and lunotriquetral ligament (line) in a patient with CPPD arthropathy
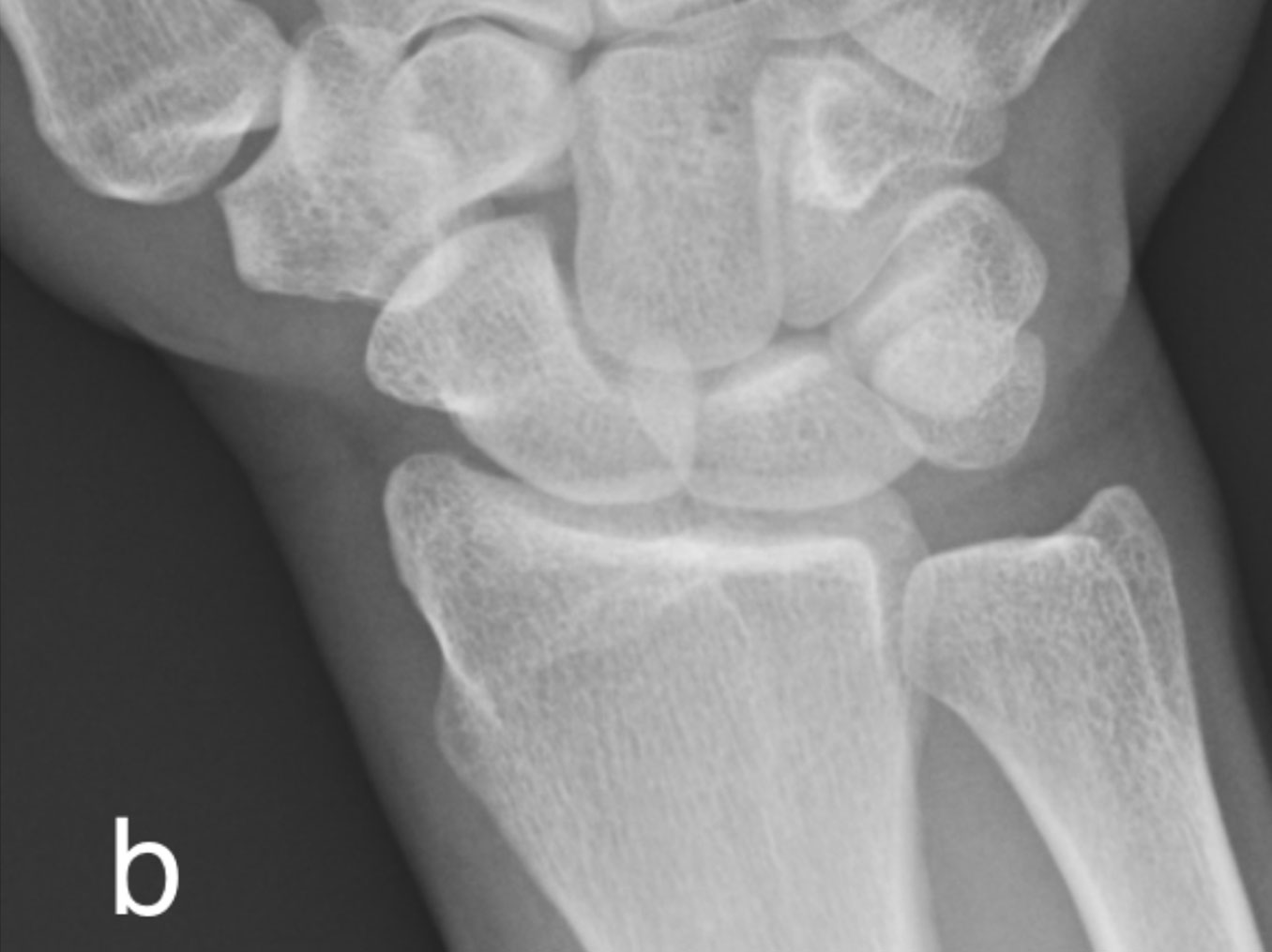 info_outline
info_outline
b) Normal radiograph for comparison
Soft Tissue Calcification
- Calcification within the soft tissues appears as a region of increased attenuation similar to bone density. It can be differentiated from heterotypic ossification/bone by the lack of a cortex and trabecular pattern which is present in the latter.
- Soft tissue calcification may occur within the cutaneous/subcutaneous tissue, in muscle or periarticular ligaments and capsular tissues.
- In the majority of cases it represents dystrophic calcification (secondary to tissue damage or injury).
- Dystrophic calcification can form in autoimmune connective tissue diseases, such as dermatomyositis and scleroderma
- Metastatic calcification occurs in conditions with raised calcium and/or phosphorus such as hyperparathyroidism, renal osteodystrophy and sarcoidosis
- Idiopathic occurs in tumoral calcinosis
Example Radiograph
 info_outline
info_outline
Extensive globular subcutaneous calcification in a patient with scleroderma
Soft Tissue Swelling
- Soft tissue swelling may be localized or diffuse
- In arthritis it is usually localized and periarticular and may be the first sign of inflammation.
- It may represent:
- soft tissue edema secondary to underlying active inflammation within a joint
- displacement of soft tissue related to an underlying joint effusion/synovitis
- it may be secondary to tendinosis and tenosynovitis.
- Findings may be subtle and include convexity to the soft tissue contour, loss of discrete fat planes and increased attenuation of the soft tissue.
- In dactylitis there is diffuse soft tissue swelling of a digit (finger or toe), also known as a sausage finger. This occurs in seronegative arthritis, most commonly psoriatic arthritis. May also occur in non-arthritis conditions including infection and sickle cell disease.
- Review the skin surface for irregularity/ulceration and soft tissue air suggesting injury or infection. Exclude radiopaque foreign bodies.
- Soft tissue swelling of increased density may represent a gouty tophus which may eventually calcify
Example Radiograph
Alignment
- Alignment must be considered with respect to both the individual joint alignment and to the general alignment of the wrist and hand.
- It is important to know the normal alignment of the wrist and hand in the different radiographic positions.
- Malalignment may be reducible and may therefore be only visible on a single projection, this is classically seen in Jaccoud’s arthropathy.
- Subluxation occurs when the articular margins are no longer 100% aligned within the normal joint range.
- In dislocation there is no remaining contact between the articular surfaces.
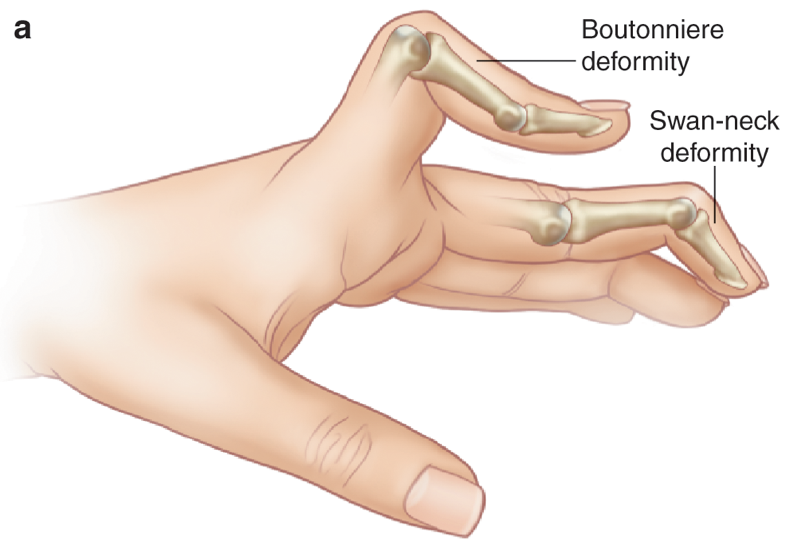
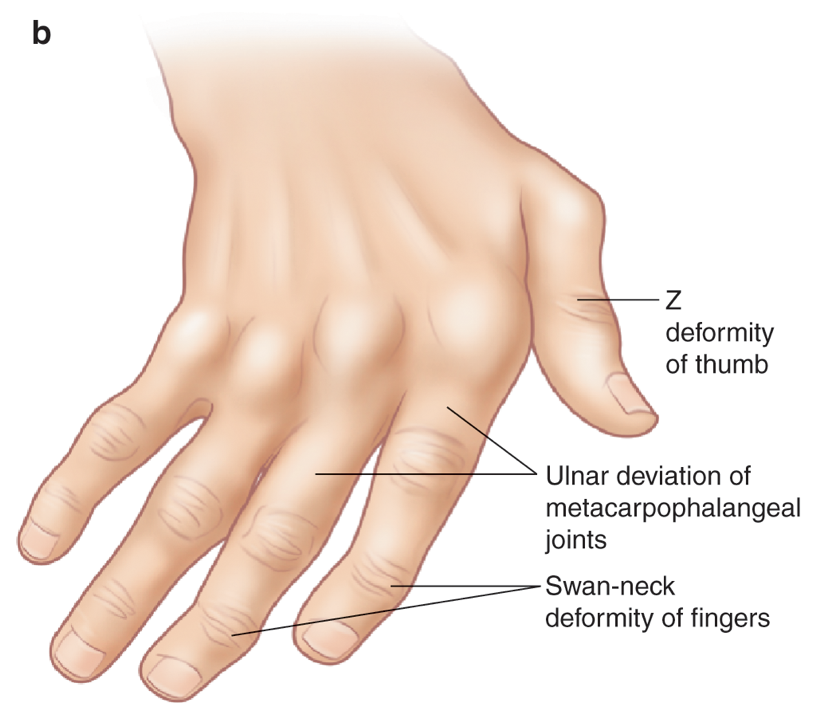
- There are variable deformities that are seen in rheumatoid arthritis, secondary to joint laxity/ligamentous and tendinous disruption, including:
- Ulnar sided deviation, commonest at the MCPJs.
- Swan neck deformity- hyperextension at PIPJ and flexion at the DIPJ
- Boutonnière deformity- hyperflexion at the PIPJ and extension at the DIPJ
- Z-deformity thumb- hyperextension at the interphalangeal joint and flexion at the 1st MCPJ
Illustrations of classical deformities in RhA
 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline