JABS
- Radiographic assessment in rheumatology requires a thorough review with an organized approach. There are many different approaches and most radiologists have their own, although similar, method of assessment. We have developed a very simple, sensible mnemonic to use when interpreting hand radiographs in rheumatology:
- JABS - Joints/Alignment/Bones/Soft Tissues
- Joints - joint space (normal, widened, narrowed-non/uniform), cortex (normal, erosions, osteophytes, subchondral cysts, sclerosis, new bone formation), pattern distribution of joint involvement (a/symmetrical)
- Alignment - normal, deviations, subluxations and dislocations, deformities
- Bone - mineralization/density, periosteal reaction, new bone formation, acro-osteolysis, fractures, bone lesions
- Soft Tissues - normal, atrophy, swelling, calcification, tophus
- Review the radiograph as a whole to get a global perspective with respect to the extent and severity of disease.
- First describe the pathology. Description is key as the use of key descriptive terminology will help you make the diagnosis e.g. erosion with overhanging edge suggests gout.
- Once we have reviewed the radiograph we need to review any previous studies to assess for interval change. Subtle changes may not be evident on comparison with the most recent exam and only become obvious when distant studies are reviewed, thus it is paramount to review back to the original available study.
- Occasionally two arthropathies may co-exist e.g. CPPD arthropathy may be co-existent with other arthropaties in up to 30% cases of patients with arthritis.
- Participating in weekly radiology-rheumatology rounds will provide an excellent insight into imaging algorithyms, diagnostics and patient management
- It is important to not try to provide an immediate diagnosis.
J - Joint
- In the rheumatology patient the dominant pathology is usually centred at the joint, hence J/Joint is where we will commence.
- We will want to compare similar joints at the same time, hence we review the DIP joints together, the PIP joints etc.This will allow us to identify subtle changes.
- Assess the joint space, is it maintained uniformly or is it widened (joint effusion/synovial thickening) or narrowed (cartilage loss)?
- Review the cortex and subchondral bone plate, are there any focal cortical defects to suggest an erosion. If there is an erosion assess it size and percentage involvement with respect to the articulating surface of the involved bone, use the additional views.
- Erosion location: central (e.g. erosive OA, psoriatic arthritis), marginal/periarticular (e.g. Rheumatoid arthritis) or juxta-articular or even remote from the joint (e.g. gout).
- Erosion margin: Sclerotic margin (thin white line deep to erosion on x-ray) occurs in gout but may also occur in inactive erosive arthropathies as a initial sign of healing with increased osteoblastic activity laying down new bone. A lucent margin to the erosion may represent active disease or early stage of inactive disease before the bone has had a chance to repair itself.
- Is there new bone formation, if so is it typical of an osteophyte (degenerative disease), enthesophyte or new bone related to a seronegative arthropathy?
- Is there periosteal reaction which would again suggest a seronegative disease in the absence of trauma or infection?
- Assess the subchondral bone, is there increased subchondral sclerosis or cyst formation to suggest degenerative disease.
A - Alignment
- If there is obvious malalignment this is where we will start. If not I will obtain a global overview and then commence my review at the distal radioulnar joint and continue distally to the distal phalanges.
- If malalignment is identified confirm it is joint centred. Exclude prior trauma.
- Describe the direction of alignment with respect to the distal component: ulnar/radial or volar/dorsal deviation.
- Is there an underlying subluxation (joint components maintain partial articulation) or dislocation (no residual articulation)?
- Is there a deformity such as swan neck, boutonniere’s or Z shaped as may occur in rheumatoid arthritis?
- Remember to review all the radiographs as reducible subluxations may not be apparent on the PA view (hands are placed on flat on table for PA radiographs which may cause reducible deformities to return to a normal alignment but recur in the oblique view e.g. Jaccound’s arthropathy).
B - Bone
- Check the bone density. Is it normal, increased (rare) or decreased (osteopenia)?
- Is it localized or generalized, unilateral or bilateral (if both hands or alternate site are available for comparison)?
- Is there a visible cause e.g.trauma related or disuse. If localized is it periarticular, what joints are involved?
- If a single joint is involved always consider infection in the differential diagnosis.
- If generalized calculate the metacarpal index (The metacarpal index (MCI), the combined cortical mid-metacarpal thickness divided by the outer mid-metacarpal diameter, can be measured for the index finger or as a combined measurement of the second to fourth digits. Values are age related but combined cortical width should be greater than 50% width mid-metacarpal, see osteoporosis section in ‘Imaging Features’)
- Assess for new bone formation and for periosteal reaction (both may occur in seronegative arthritis) and for subperiosteal resorption (e.g. hyperparathyroidism)
- Increased bone density may occur with avascular necrosis, e.g. Kienbock’s disease of the lunate and may go on to osseous collapse.
- Assess phalangeal tufts for acro-osteolysis, bone resorption distal phalanges. This has a wide differential including scleroderma and Raynaud’s
S - Soft Tissues
- There may be localized or diffuse swelling or atrophy of the soft tissues.
- Check for loss or deviation of the normal soft tissue fat planes. Is there any change in the contour of the skin? These changes usually point to localized soft tissue pathology e.g. soft tissue swelling on the medial margin of the ulnar styloid suggest tendinous and/or tenosynovitis of the ECU, commonly seen in Rheumatoid arthritis.
- Is there swelling overlying a joint suggesting an underlying joint effusion/synovitis. This will alert me to closely review this joint for pathology.
- Is there generalized swelling of an entire digit, dactylitis? This may suggest infection or seonegative disease such as psoriatic arthropathy.
- Soft tissue loss, particularly distally would suggest scleroderma.
- Is there soft tissue calcification, is it within expected location of a tendon (calcific tendinosis in hydroxyapatite disease), or evidence of calcinosis cutis e.g. SLE?
- Vascular calcification distally extending to the hands is uncommon and is usually suggestive of chronic diabetes or chronic renal disease. Assess for changes of hyperparathyroidism.
- Exclude soft tissue air, ulcers and radiodense foreign bodies all of which may indicate the presence of infection.
Common Sites Involvement Of The Major Arthritides
Osteoarthritis (Primary)
- Typical distribution of affected joints and the subsequent pattern recognition are key elements in helping the clinician arrive at a diagnosis.
- DIPJs, PIPJs, and the first CMCJ are classically associated with primary OA. If other joints of the hand are involved with OA, one should think of secondary causes to include crystal disease, RA, and trauma.
- The second and third MCPJs are an unusual site of primary OA and, if noted, should prompt one to think about CPPD and more importantly its associated etiologies such as hemochromatosis (which shouldn’t be missed).
Other Joints
- Symmetrical involvement of the PIP, MCP, and wrist joints (symmetry is a key feature in that both hands are involved rather than perfect symmetry).
- Erosive osteoarthritis is a subset of primary OA and predominantly involves the hands.
- The PIP and DIP joints are more commonly involved although any of the above joints in primary OA may be involved.
- There are bony outgrowths at the joint margins, joint space loss, and central erosions. The latter produces the “seagull” appearance.
- The disease may progress with eventual ankylosis.
- The lack of marginal erosions, periosteal reaction, and new bone formation, other than osteophytes, helps to separate the disease from psoriatic arthropathy.
Erosive osteoarthritis
 info_outline
info_outline
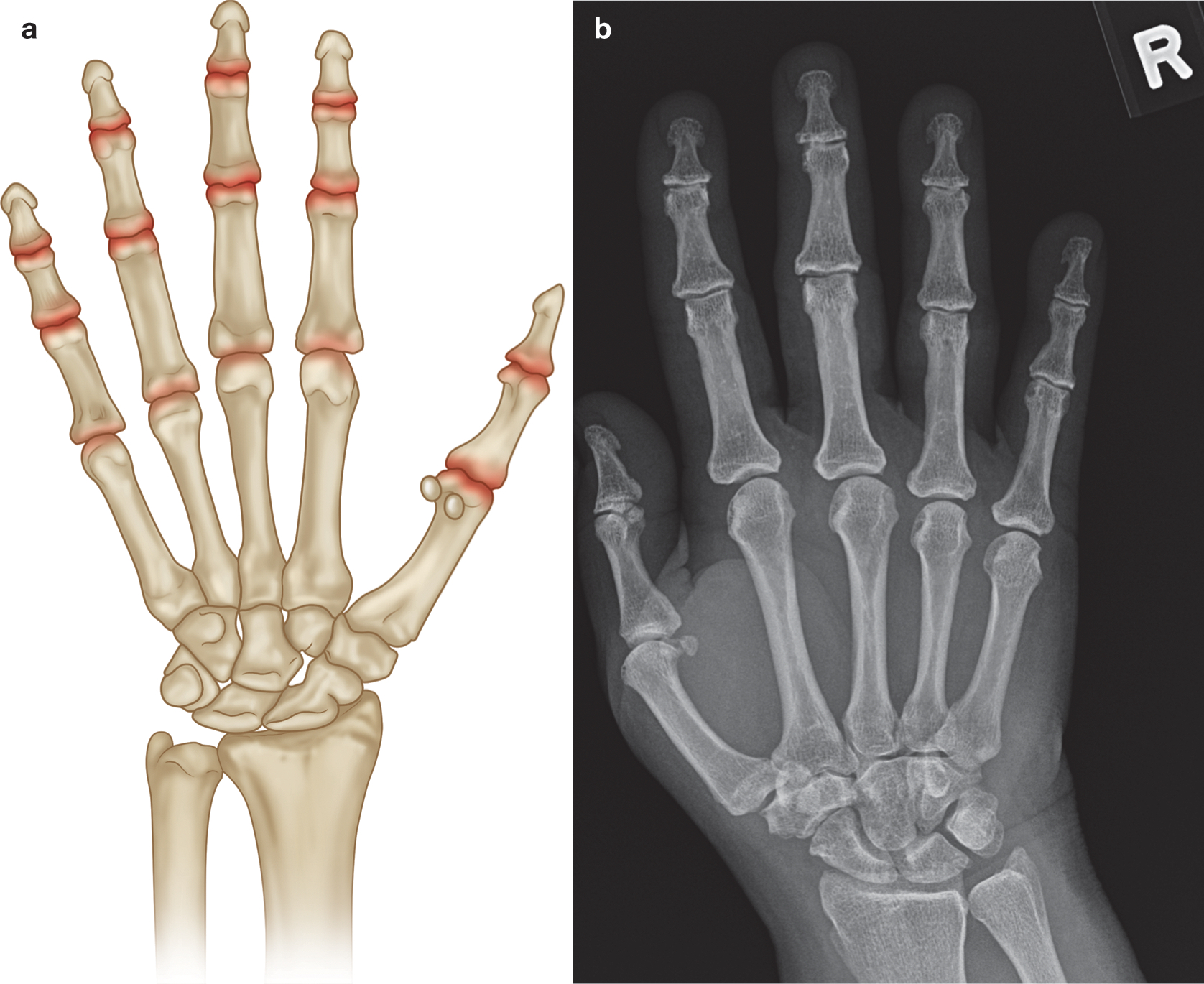
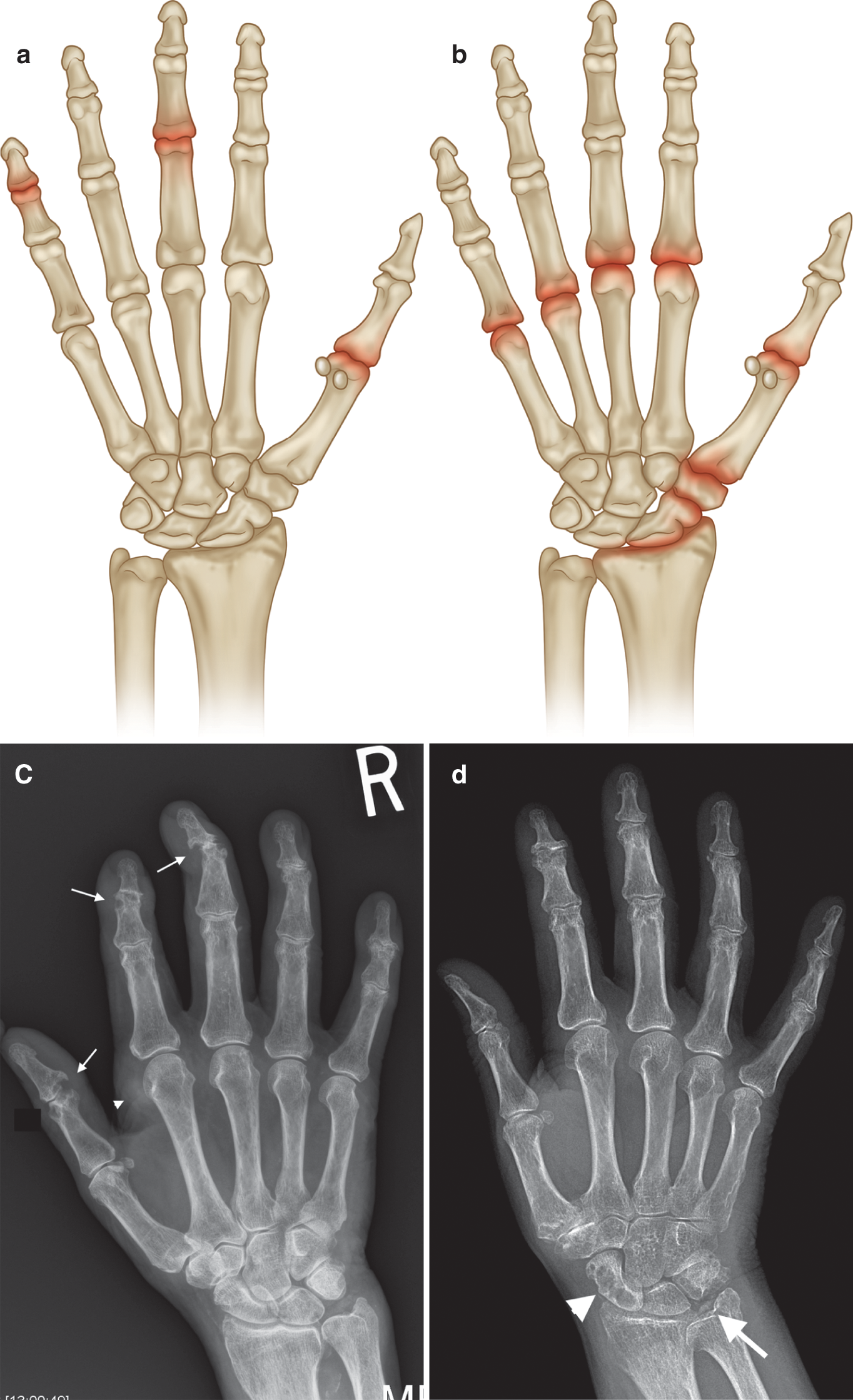
(a) Common sites of involvement with osteoarthritis of the hand (highlighted in red). (b) PA radiograph of right hand with early osteoarthritis demonstrating joint space loss at the PIP and DIP joints and early subchondral cysts at the second and third
 info_outline
info_outline
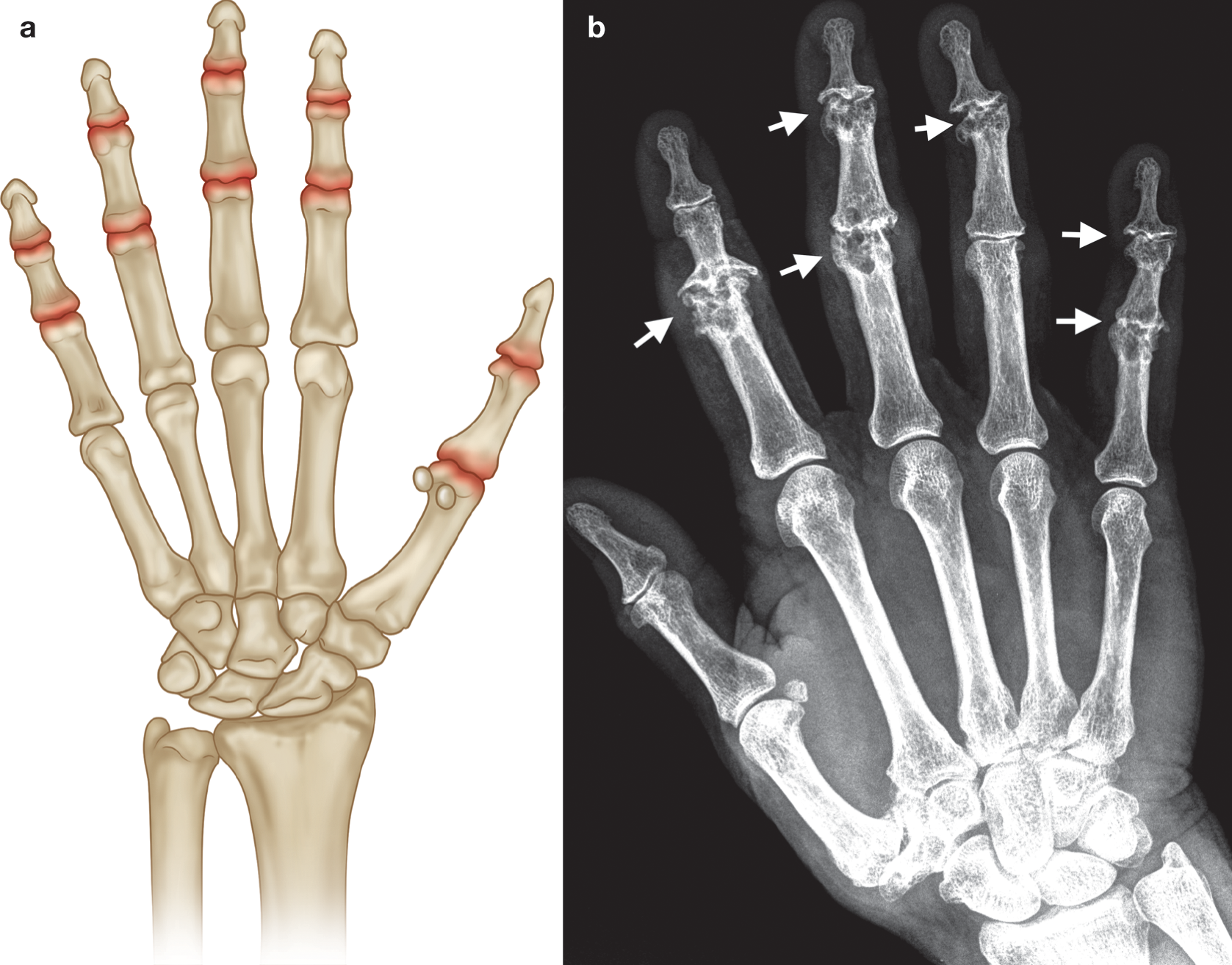
(a) Common sites of involvement with erosive osteoarthritis of the hand. (b) PA radiograph of right hand with changes of chronic erosive osteoarthritis at the PIP and DIP joints (arrows) with classic central erosions and “gull wing” osteophytes (most
Rheumatoid Arthritis
Hands
- Symmetrical involvement of the PIP, MCP, and wrist joints (symmetry is a key feature in that both hands are involved rather than perfect symmetry).
- Feet are also involved in RA with similar joints being involved, i.e. PIP and MTP joints. The fifth metatarsal head is a common first site of erosion.
Other Joints
- Elbows, glenohumeral, cervical spine, hips, knees, and ankles are the most common involved joints in RA.
- Note that lumbar spine is almost never involved. Again symmetry is typical but perfect symmetry is not absolute.
 info_outline
info_outline
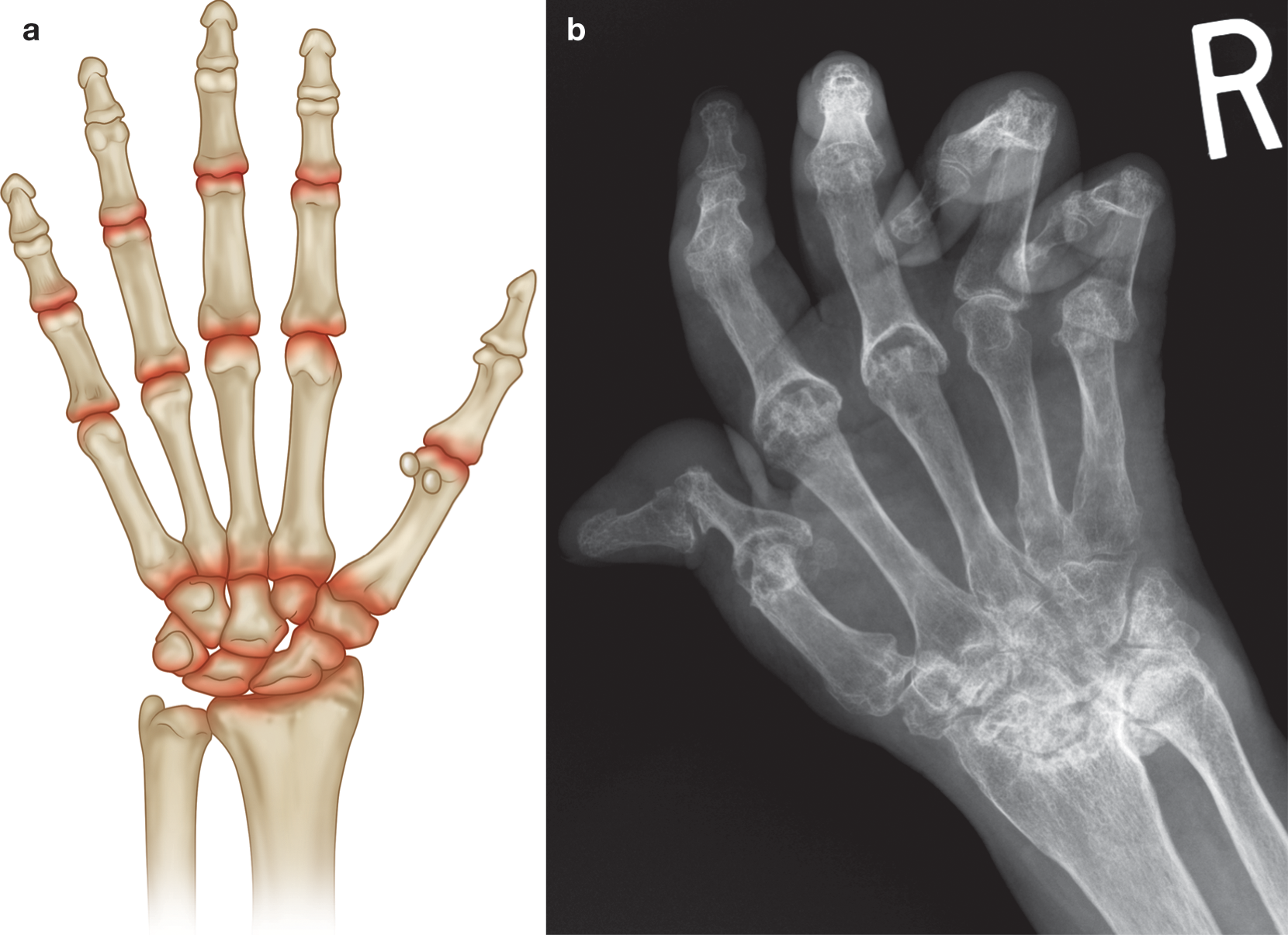
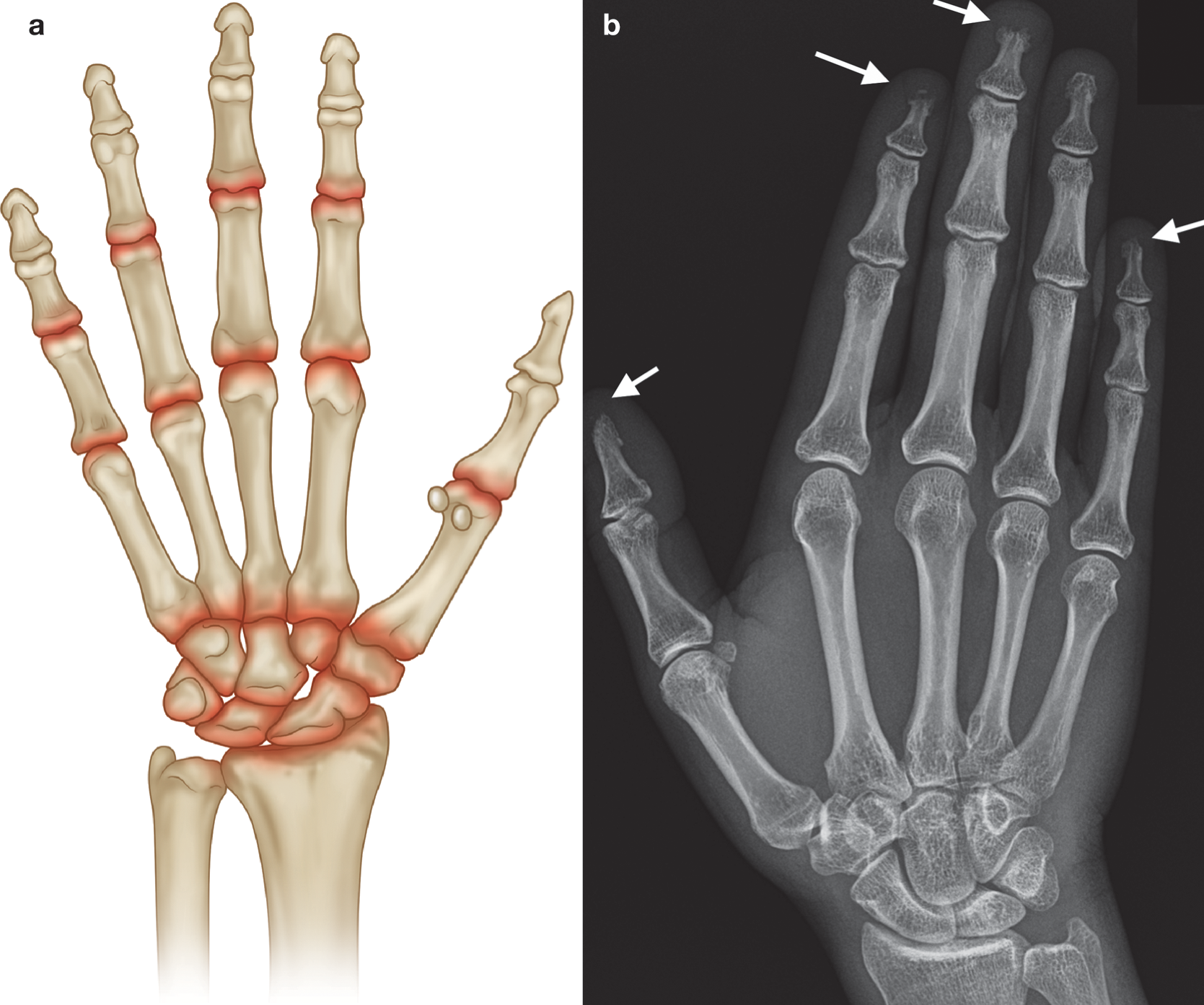
(a) Common sites of involvement with rheuma- toid arthritis. (b) PA radiograph of right hand with changes of long-standing rheumatoid arthritis (similar changes were noted in the left hand and wrist in keeping with sym- metrical disease). Marked diffuse osteopenia, extensive erosions at radioulnar joint, partial collapse at proximal carpal row, erosions at the MCPJs and first IP joint, “Z” shaped deformity in the thumb, subluxation at the fifth MCPJ, and flexion deformities at the PIPJs
Seronegative Arthritis
(Ankylosing Spondylitis, Reactive Arthritis, Psoriatic Arthritis, Enteropathic Arthritis)
Hands
- Several patterns can be found in PsA, in particular the distal form (DIP involvement) and the symmetric polyarthritis pattern that can mimic RA (PIP, MCP, and wrist involvement).
- Periarticular osteopenia occurring in RA and periostitis (laying down of new bone) occurring in PsA are helpful in differentiating RA from PsA.
Other Joints
- All seronegative arthritides can affect the sacroiliac joints (SI).
- AS by definition involves the sacroiliac joints symmetrically, whereas the other types may affect SI joints asymmetrically
- Lumbar and thoracic spine are involved, but cervical spine is less commonly involved, with the exception of PsA
- Lower extremity asymmetric large joint oligoarthritis is classic and is found in the hip, knee, and ankle joints
 info_outline
info_outline
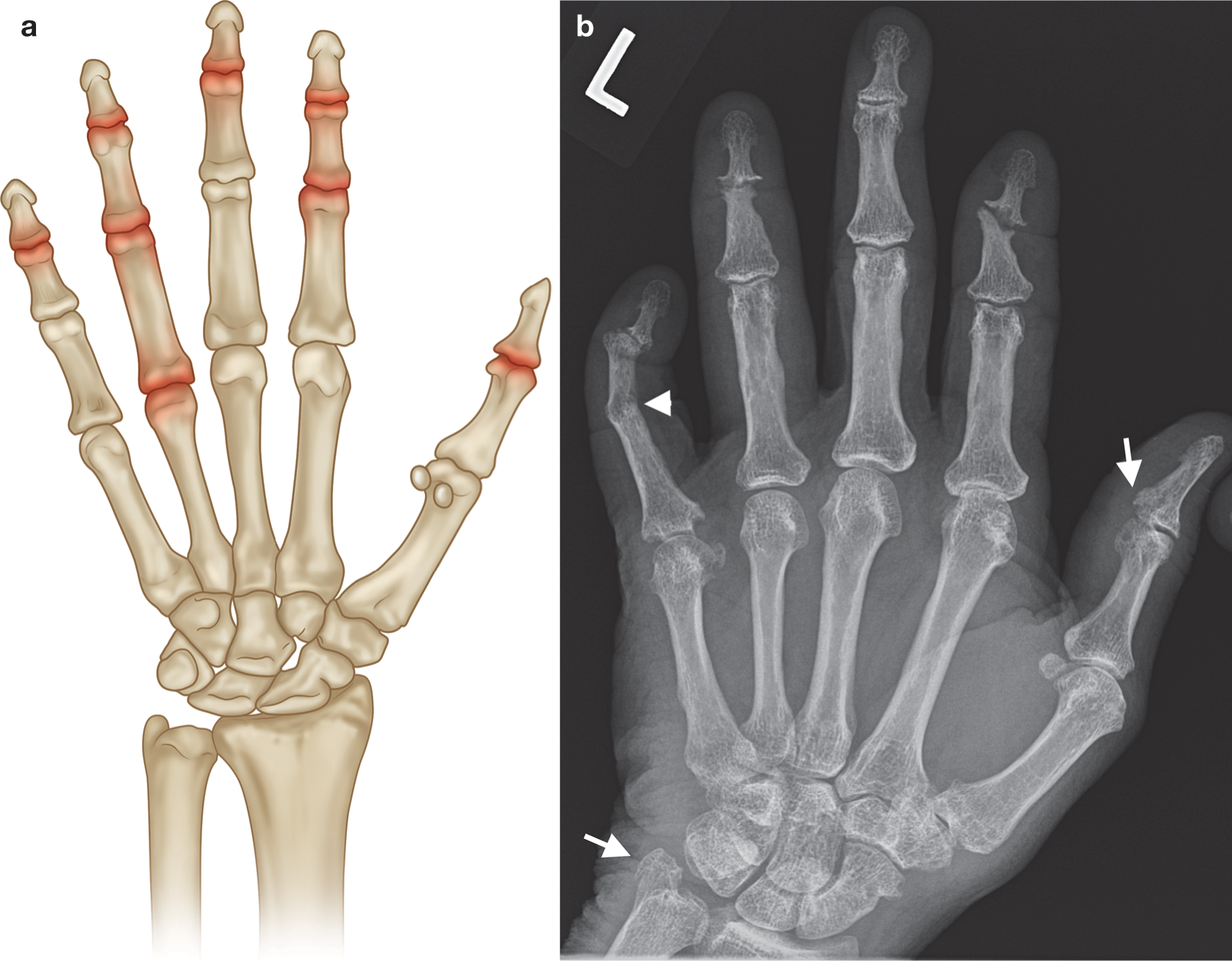
(a) Common sites of involvement with seronegative arthritis. (b) PA radiograph of the left hand in a patient with long-standing psoriatic arthritis (asymmetrical changes were present on the right hand). Normal bone density, new bone formation at ulnar styloid and base of the first distal phalanx (arrows), marginal erosions at the distal scaphoid and the fifth MCPJ and DIPJ, central and marginal erosions at the second and fourth DIPJs, and joint fusion at the fifth PIPJ ( arrowhead ). gouty tophus ( arrowhead). Note absence of periarticular osteopenia. There was asymmetrical left hand involvement (not shown). d ) PA radiograph of the right hand with chondrocalcinosis triangular fibrocartilage ( arrow ), normal bone density, mild joint space loss at the MCPJs, moderate degenerative changes at the first CMC, and crystal-related prominent subchondral cysts of the scaphoid. Incidental mild osteoarthritis, age-related, at the PIP and DIP joints in ( c ,d )
Crystalline Arthropathies
(Gout, CPPD)
Hands
- Any joints of the hands can be affected in gout or CPPD arthropathy.
- When these diseases become chronic and recurrent, they often mimic rheumatoid arthritis.
- In the case of CPPD, this clinical presentation is termed pseudo-rheumatoid arthritis.
- Plain radiographs would be of great help especially if it shows OA of the second and third MCPs as well as calcification in the cartilage of the triangular fibrocartilage complex (TFCC) of the wrist.
Other Joints
- Almost any other joints can be involved in crys- talline arthropathies, but involvement of the spine, except for atlantoaxial joint, is unusual
- The first MTP is classically the first joint to be involved in gout (podagra).
 info_outline
info_outline
Common sites of involvement with (a) gout and (b) CPPD arthropathy. (c) PA radiograph of the right hand in a patient with a 15-year history of gout and chronic renal failure with marginal erosions (arrows), some with overhanging edges (first IPJ), and
Connective Tissue Disorders
(SLE/ Scleroderma/Polymyositis/ Dermatomyositis/Sjogren’s)
Hands
- SLE often involves the hands in the typical RA distribution (PIPs, MCPs, and wrists) and can have the same deformities as RA (swan neck and boutonnière), but the lack of erosions on plain radiographs is a key differentiating factor in long-standing disease.
- The pattern of reversible joint deformity is termed Jaccoud arthropathy.
 info_outline
info_outline
(a) Common sites of involvement with connective tissue disease. (b) PA radiograph of the right hand with scleroderma demonstrating resorption at phalangeal tufts (arrows), acro-osteolysis. No significant overlying soft tissue atrophy or soft tissue calcification