Edema & Osteitis
- Edema is an excess accumulation of fluid in the bodies tissue and can occur from multiple causes.
- With respect to SpA we will focus on edema related to inflammation.In the case of bone this inflammatory changes is called osteitis.
- Enthesitis and capsulitis are relate to inflammatory changes and edema at ligament or tendon attachment to bone and joint capsule respectively
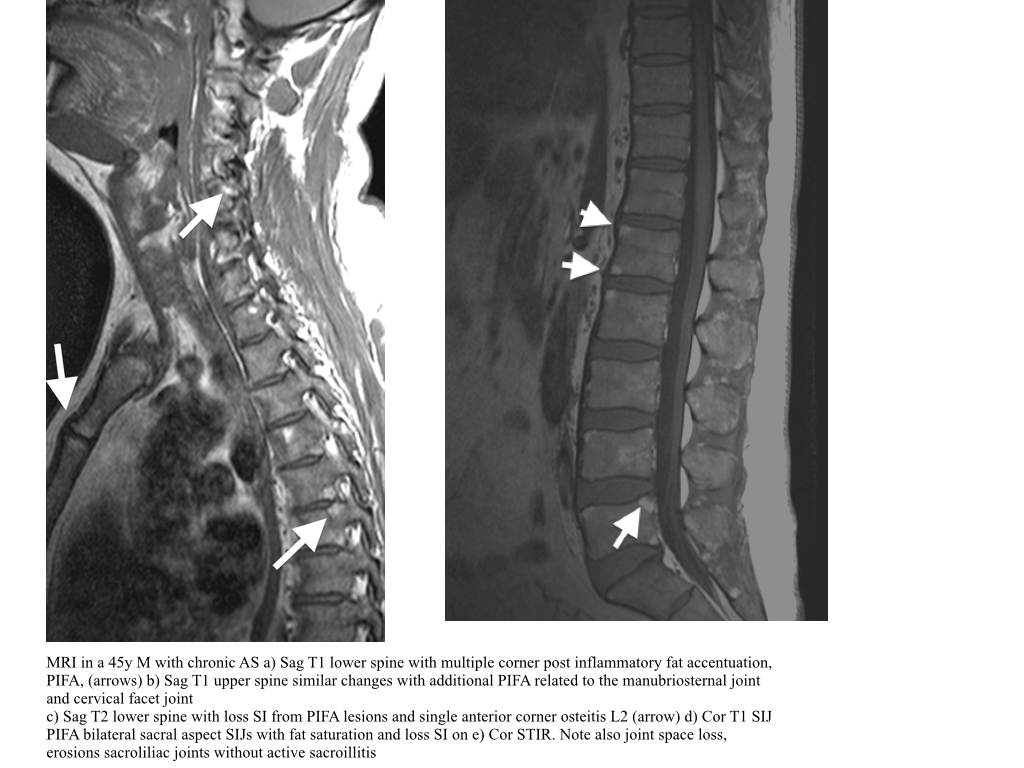
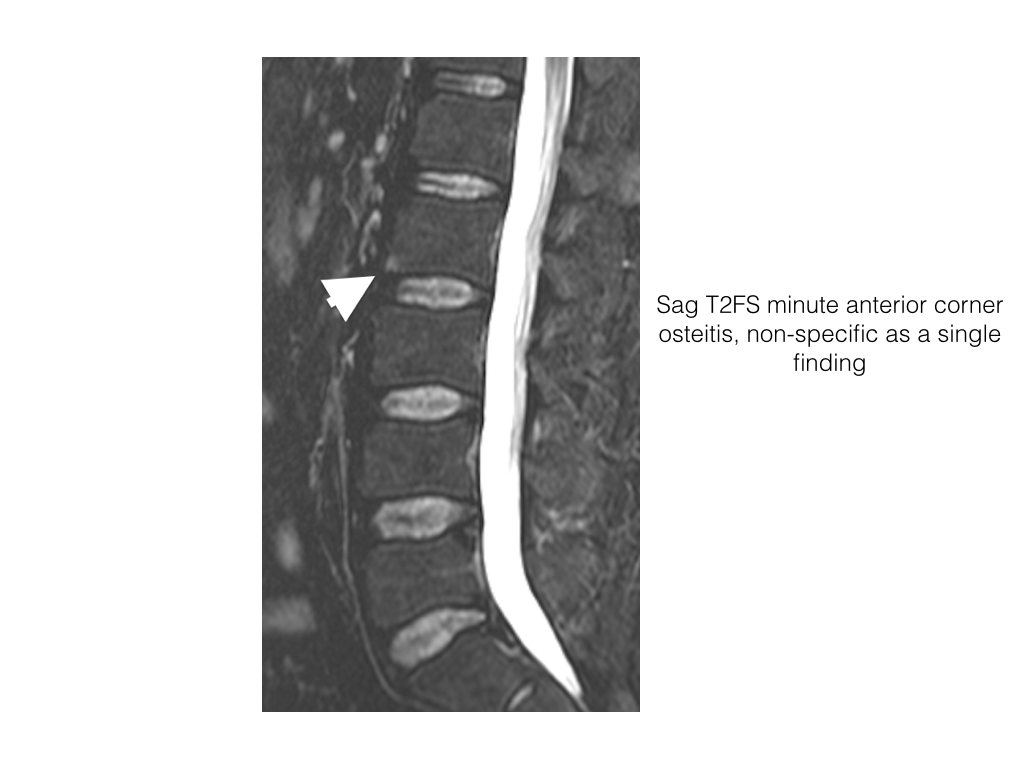
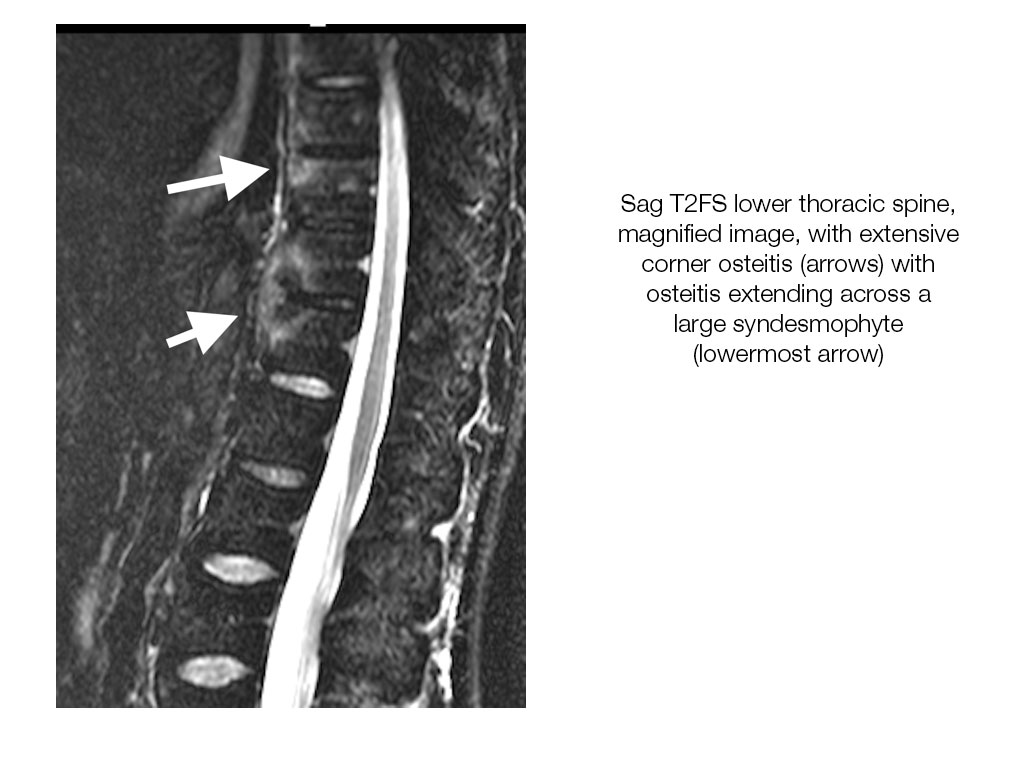
Osteitis-Spine
- MRI can demonstrate focal osteitis, high SI on STIR, low on T1, at the anterior corners vertebral body in the acute stage. This is also termed a corner inflammatory lesion. These may occur anteriorly or posteriorly.
- Non-corner inflammatory lesions are identified as osteitis parallel to the endplate centrally. When osteitis involves the more lateral margins of the vertebral body, at the level pedicles and beyond, it is termed a lateral inflammatory lesion.
- Osteitis at the costovertebral and costotransverse articulations may occur and are thought to be more sensitive indications of SpA.
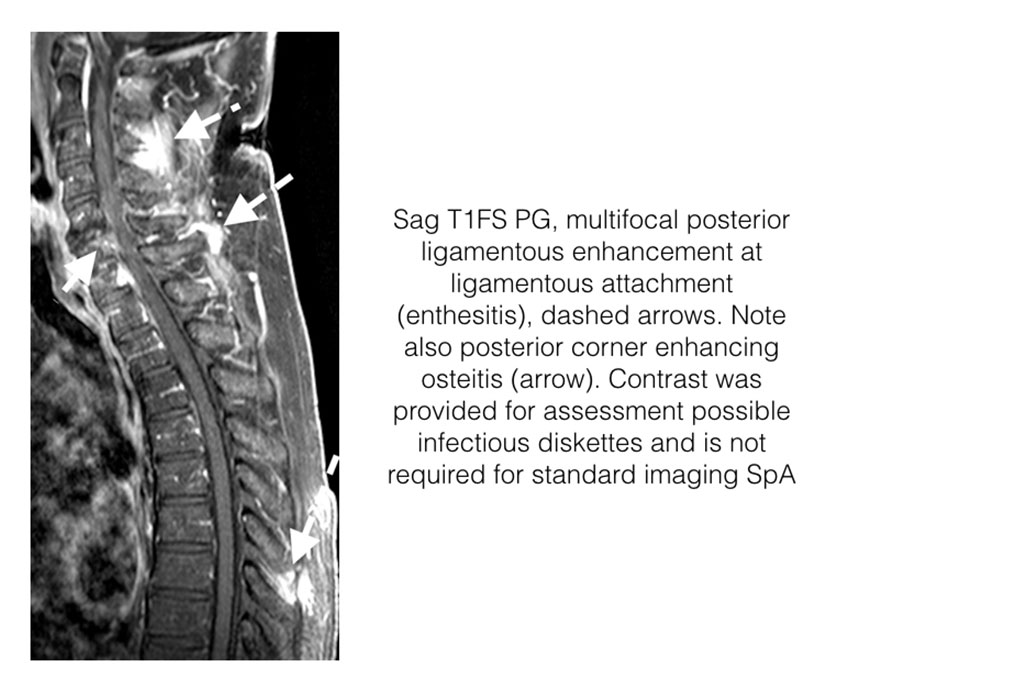
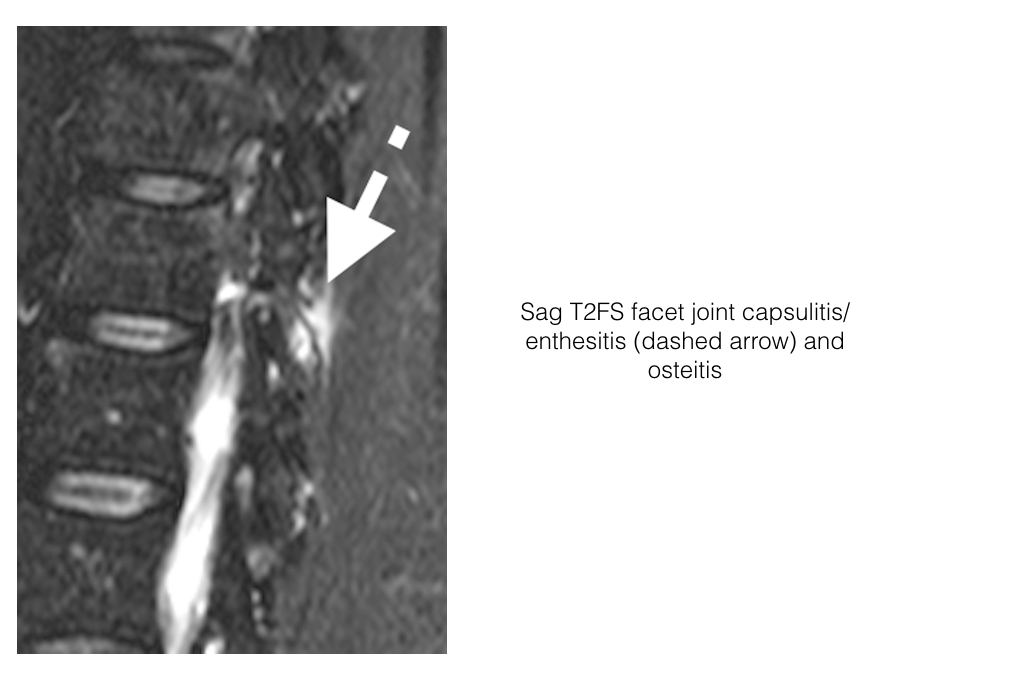
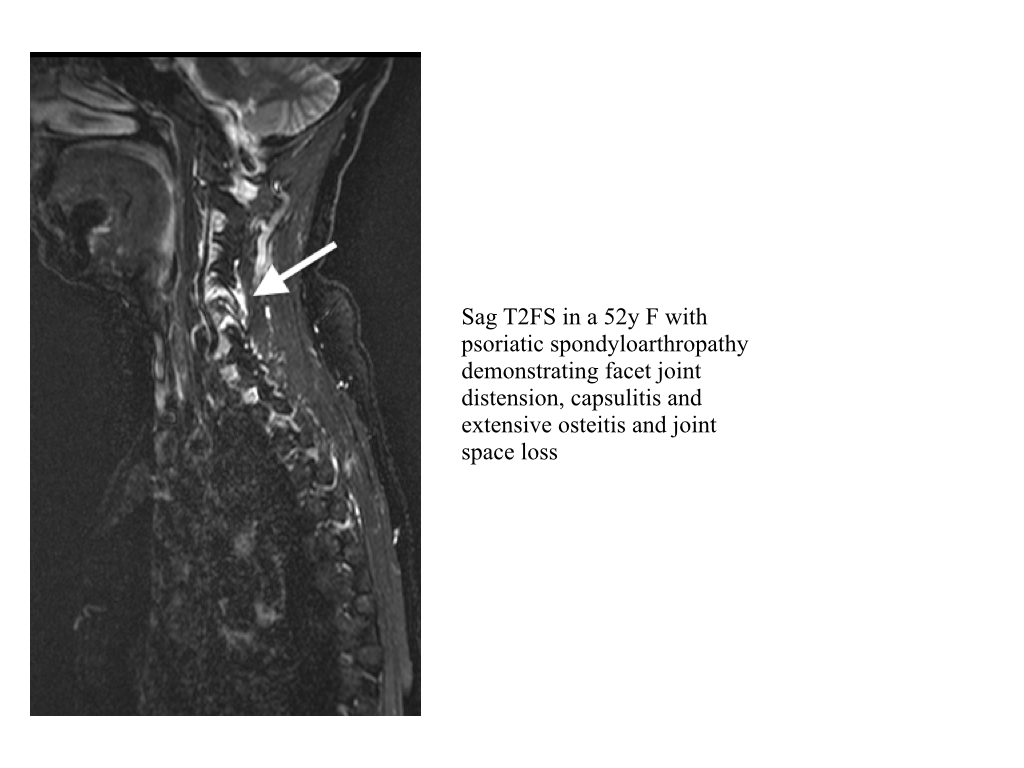
- Inflammation may also involve the posterior elements of the vertebra including the facet joints (including capsule, facets and perifacet soft tissues) and posterior ligaments (entheses).
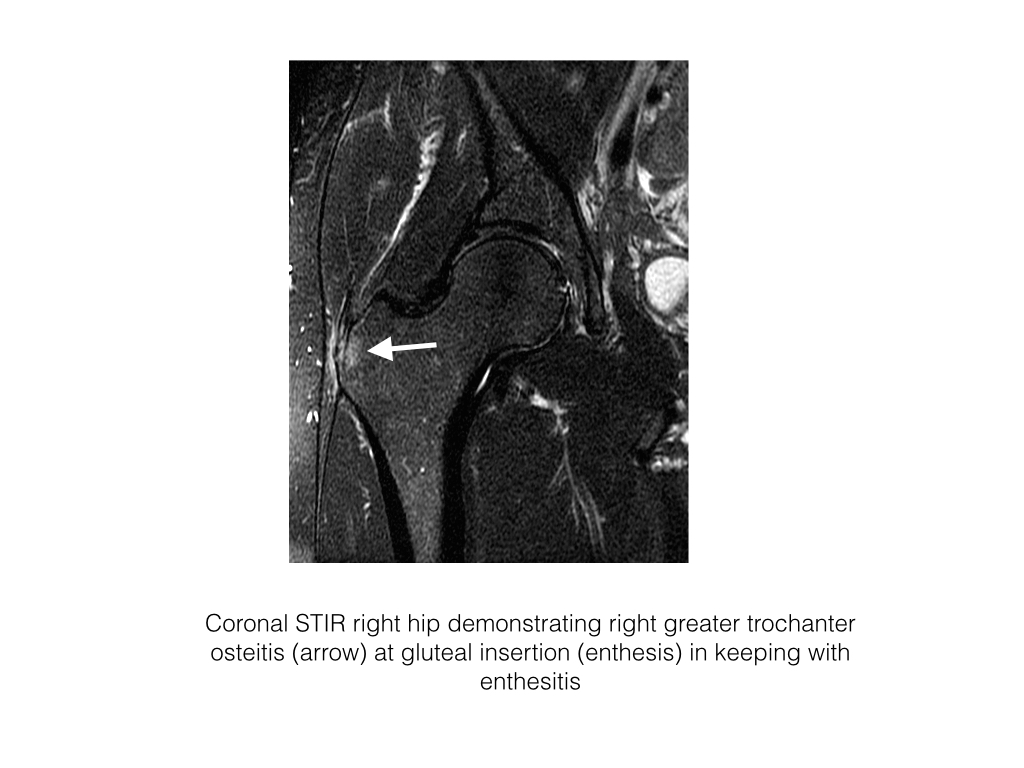
Enthesitis
- Enthesitis is the inflammation of the enthesis, site of insertion of tendon, ligament or joint capsule to bone.
- There are 2 types of entheses, fibrous and fibrocartilaginous
- Enthesitis is common in SpA. It may be subclinical and detected only on imaging.
- On MRI enthesitis is identified as high signal intensity on STIR or contrast enhanced T1FS at the site of ligament, tendon or capsular attachment to bone.
- Ultrasound is not used clinically in the assessment of axial enthesitis due to the depth of tissue and the availability of MRI.
- CT can not assess osteitis or enthesitis.
- Nuclear studies with bone scan would demonstrate increase uptake at sites of osteitis but is non-discriminatory, is not as sensitive as MRI and incurs a significant radiation dose.
Enthesitis-Spine
- With respect to the Spine, enthesitis is more common posteriorly at ligamentous insertion, supraspinous and interspinous ligaments, facet joint capsule, and paravertebral muscle tendinous insertions.
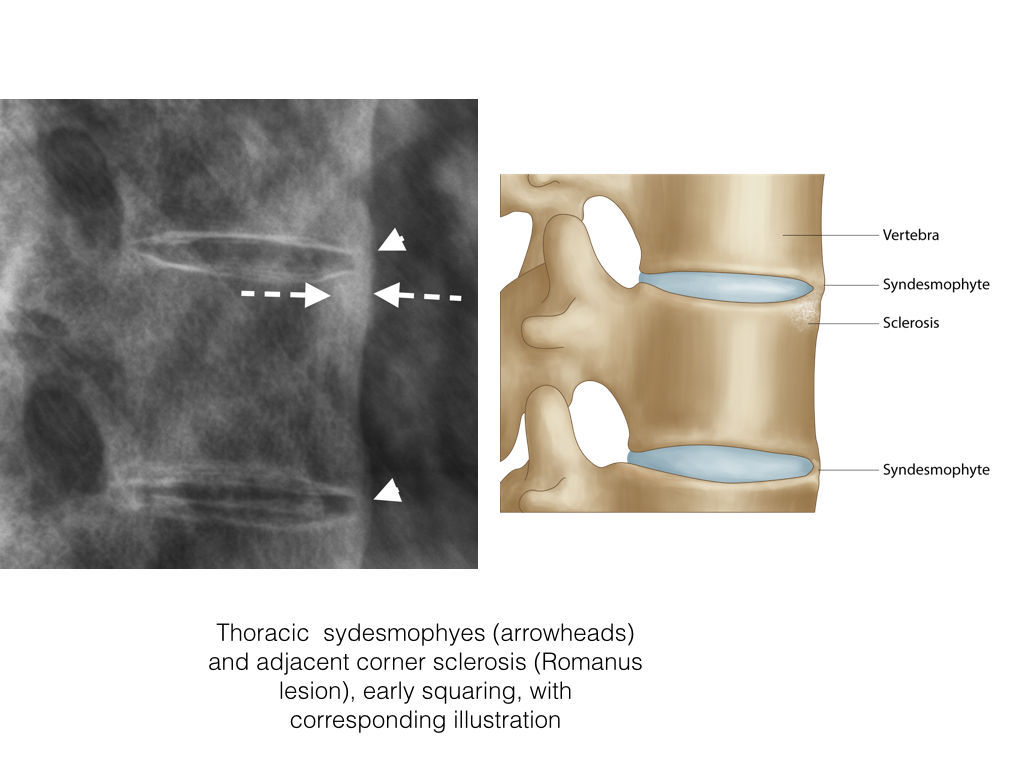
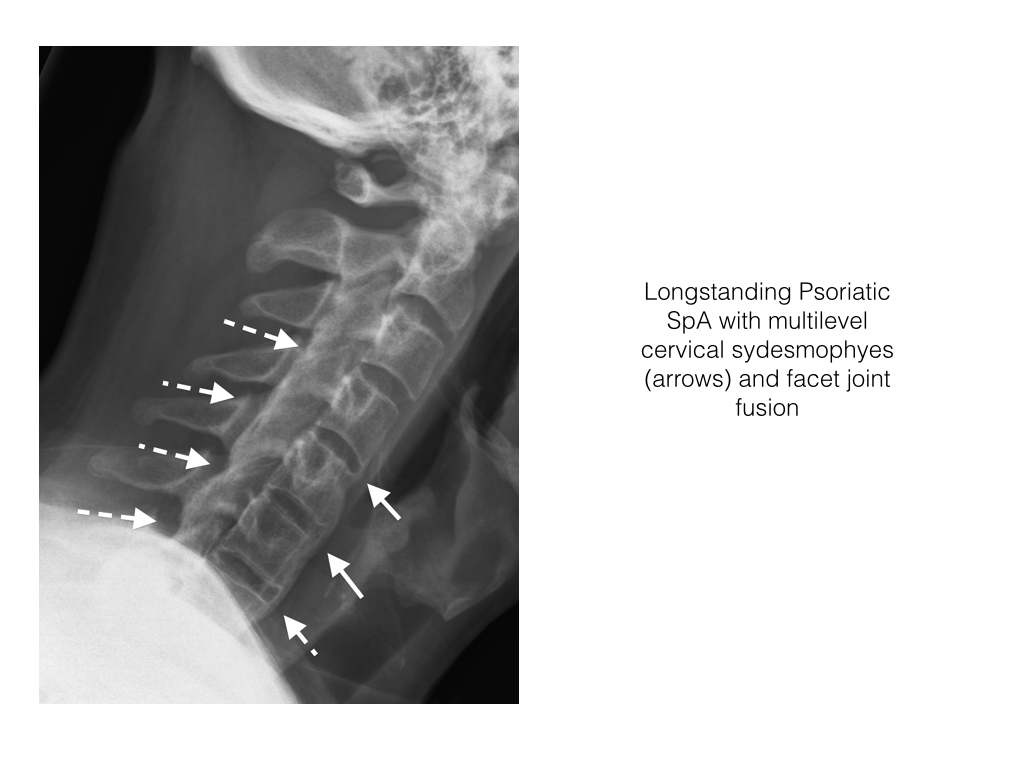
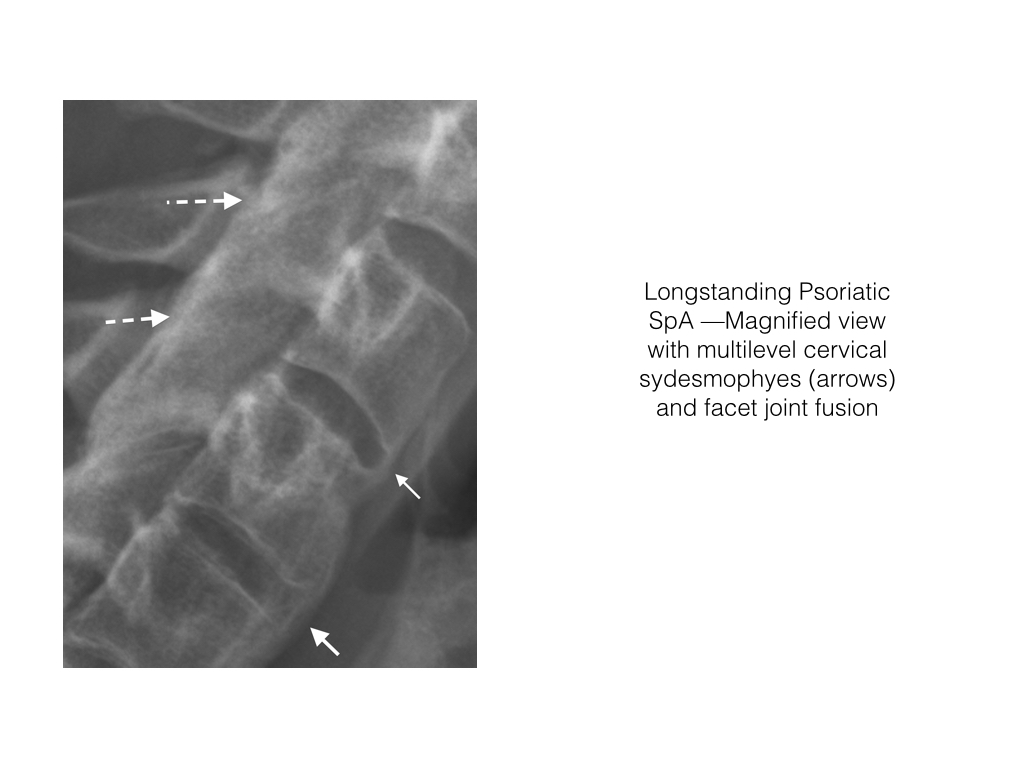
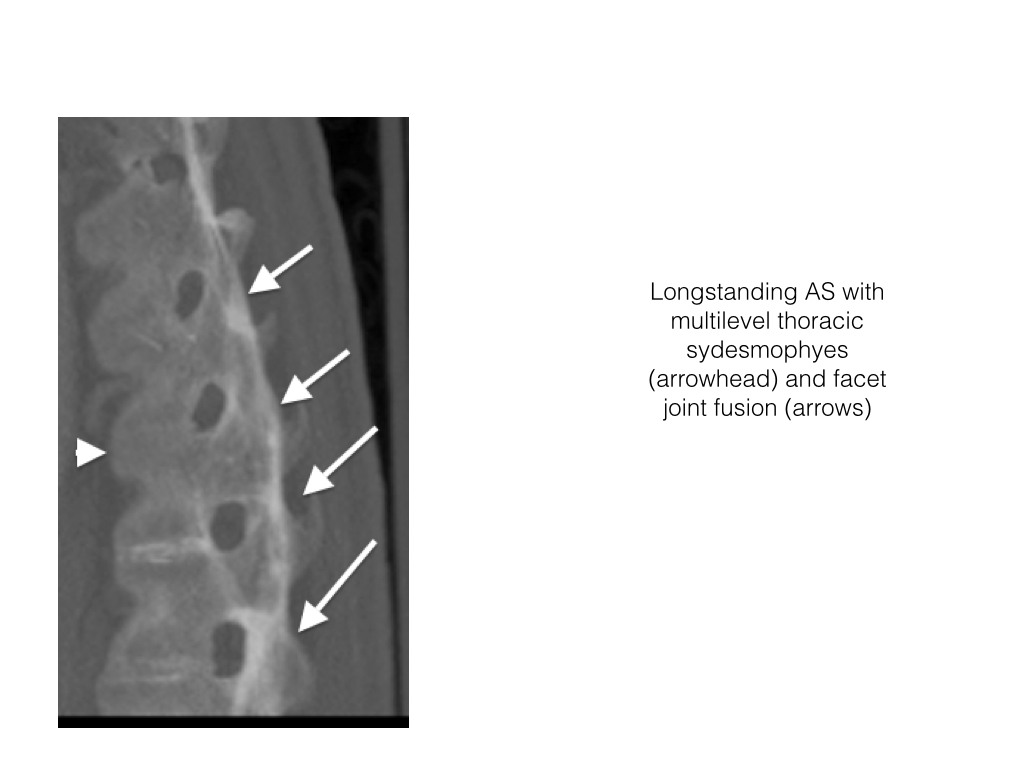
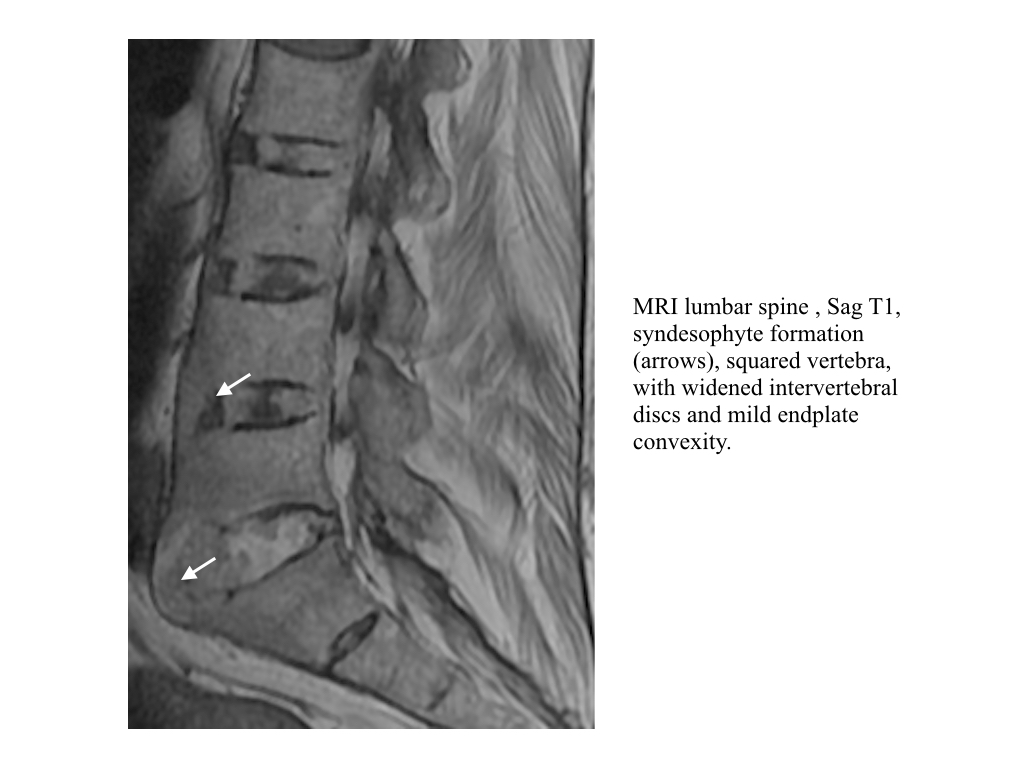
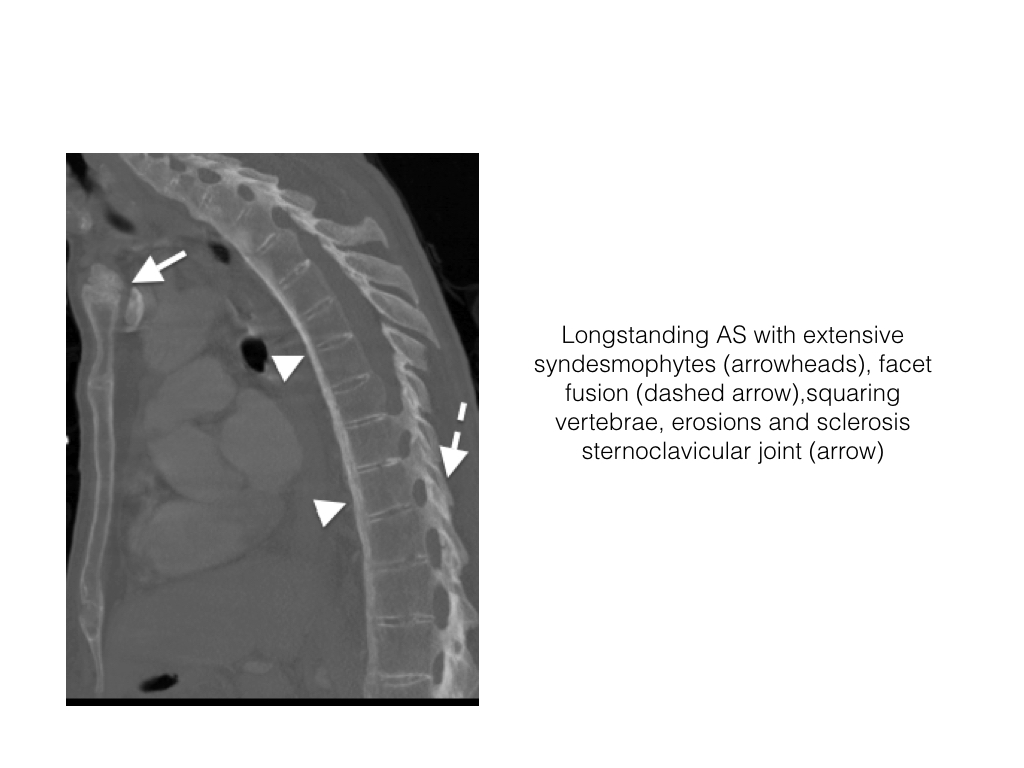
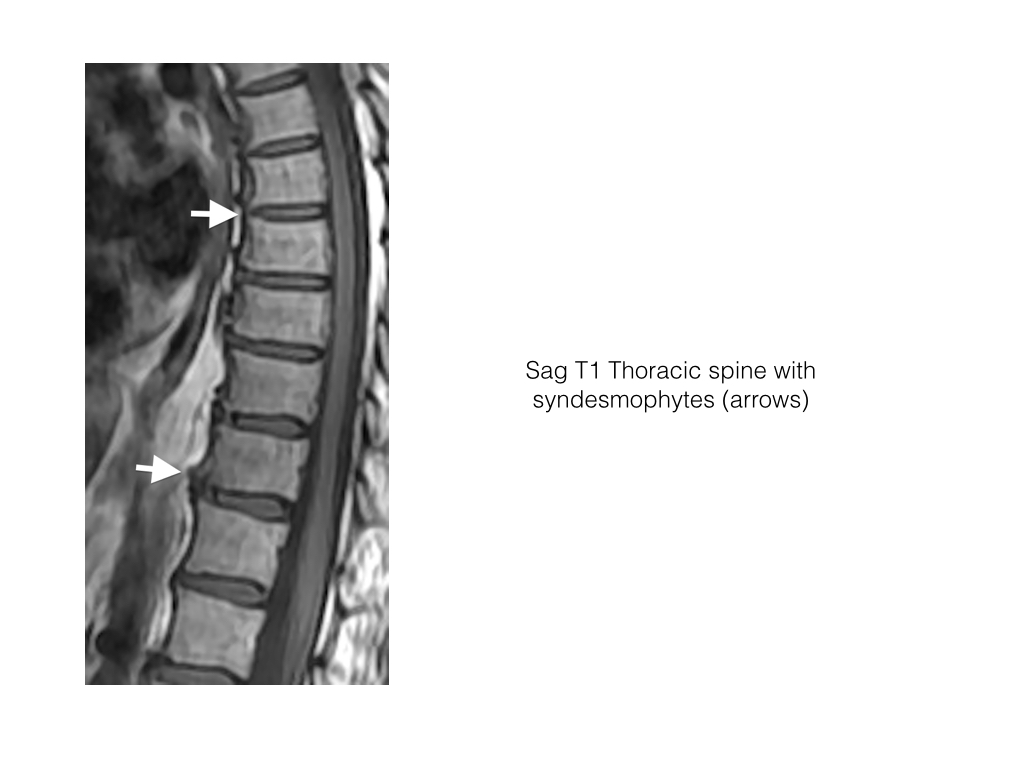
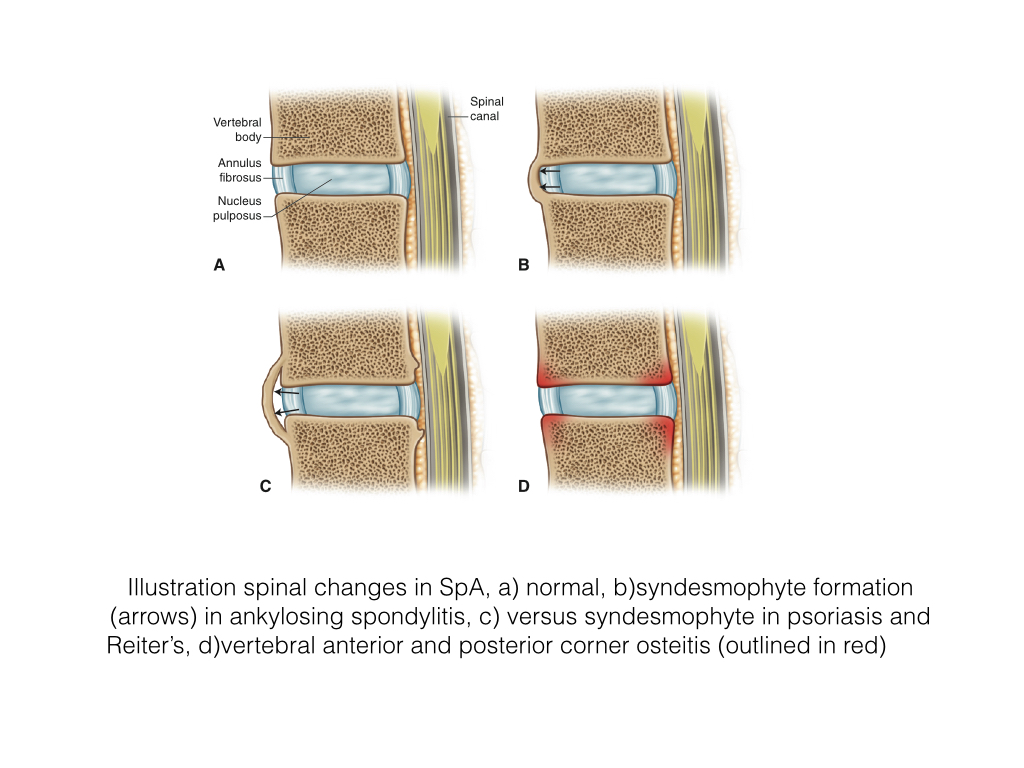
Syndesmophytes
- A syndesmophyte is new bone formation within the outer fibres of the annulus fibrosis of the intervertebral disc commencing at the juncture with the vertebral body, sharpey’s fibres.
- Ankylosing spondylitis patients are particularly prone to developing syndesmophytes.
- Bone growth eventually forms a bridge between the involved vertebral bodies. They are most pronounced at the anterior and lateral margins of the vertebral body.
- This is a late finding in the disease; approximately 25% of patients will demonstrate syndesmophytes by 10 years and 65% by 20yrs of disease
- Syndesmophytes are best visualized on CT and radiographs.
- MRI is less sensitive due to a larger acquired field of view and decreased resolution.
- Sag T1 is more sensitive than STIR in assessing syndesmophytes
- Need to be differentiated from DISH where the anterior longitudinal ligament is ossified and extends over the anterior vertebral body, requires involvement of 4 adjacent vertebrae for a diagnosis of DISH.
- Endplate osteophytes are more triangular in nature and grow outwards.
- Psoriasis and Reiter’s related paravertebral ossification begins proximal to the juncture of the intervertebral disc and vertebra.
Romanus Lesion
- A Romanus lesion, initially described on radiographs as an early spinal change in AS, is an erosion of a vertebral corner at the discovertebral junction
- It represents small erosions at the superior and inferior endplates (corners on lateral radiograph) of the vertebral bodies, with surrounding reactive sclerosis. Eventually the vertebral bodies become squared.
- On a radiograph anterior vertebral body corner erosion can be seen. May heal with sclerosis, the “shiny corner”.
- With an MRI, Focal osteitis can be seen as high SI on STIR, and low SI onT1, in the anterior corners vertebral body i.e. Anterior corner osteitis
- Chronic lesions are depicted as foci of fat signal intensity, high on T1 and T2, i.e PIFA.
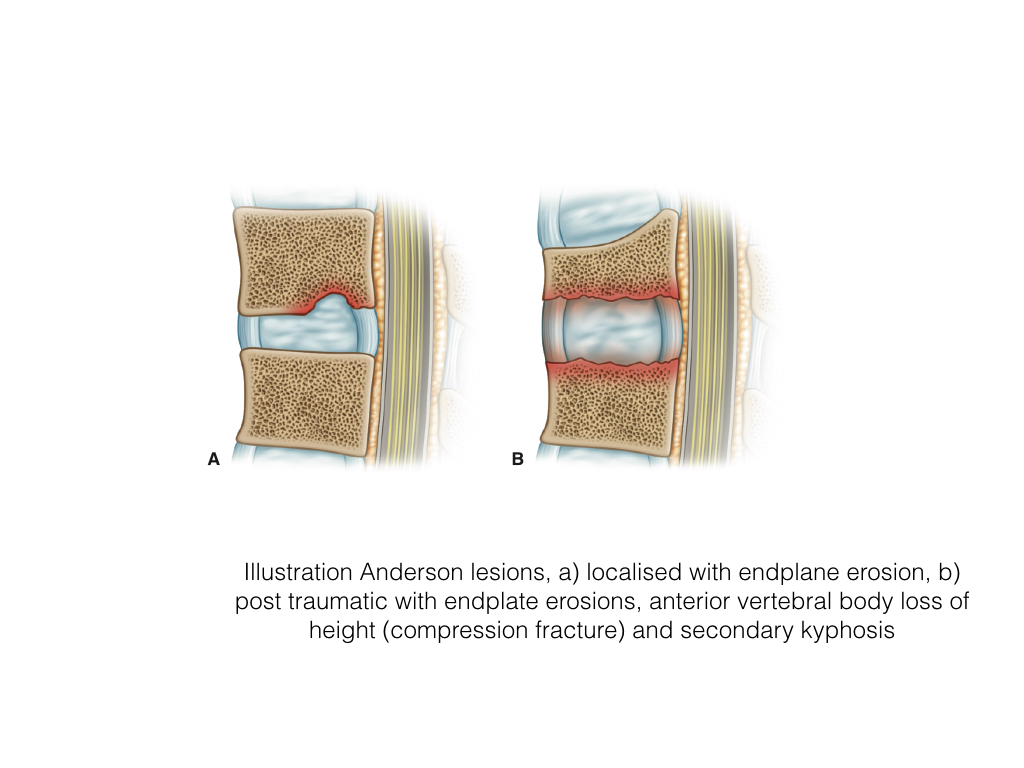
Andersson Lesion
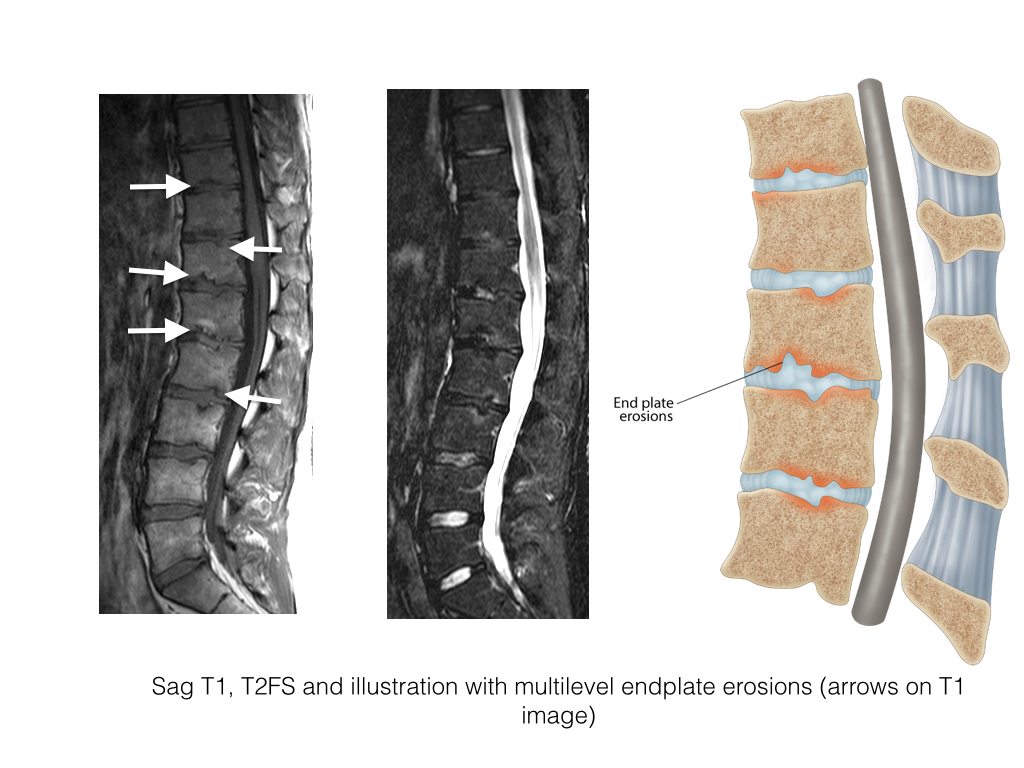
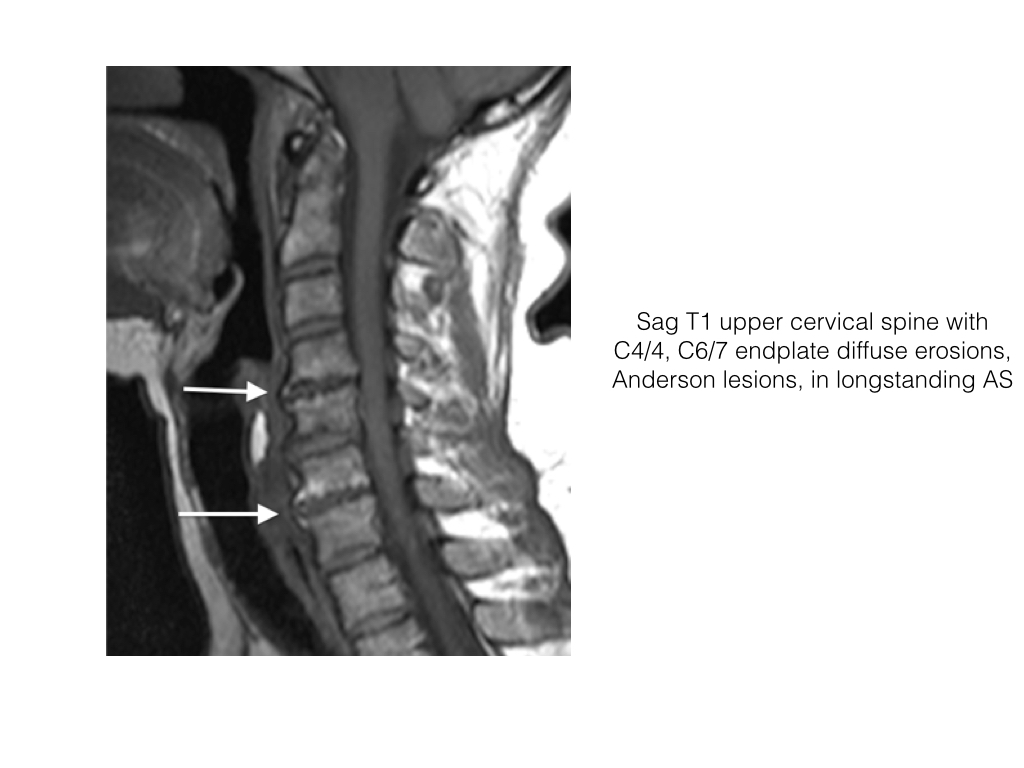
- Spondylodiscitis, or Andersson lesion, is the occurrence of discovertebral erosions in patients with SpA
- Lesions may be localised or diffuse.
- The localised lesion may be central or peripheral.
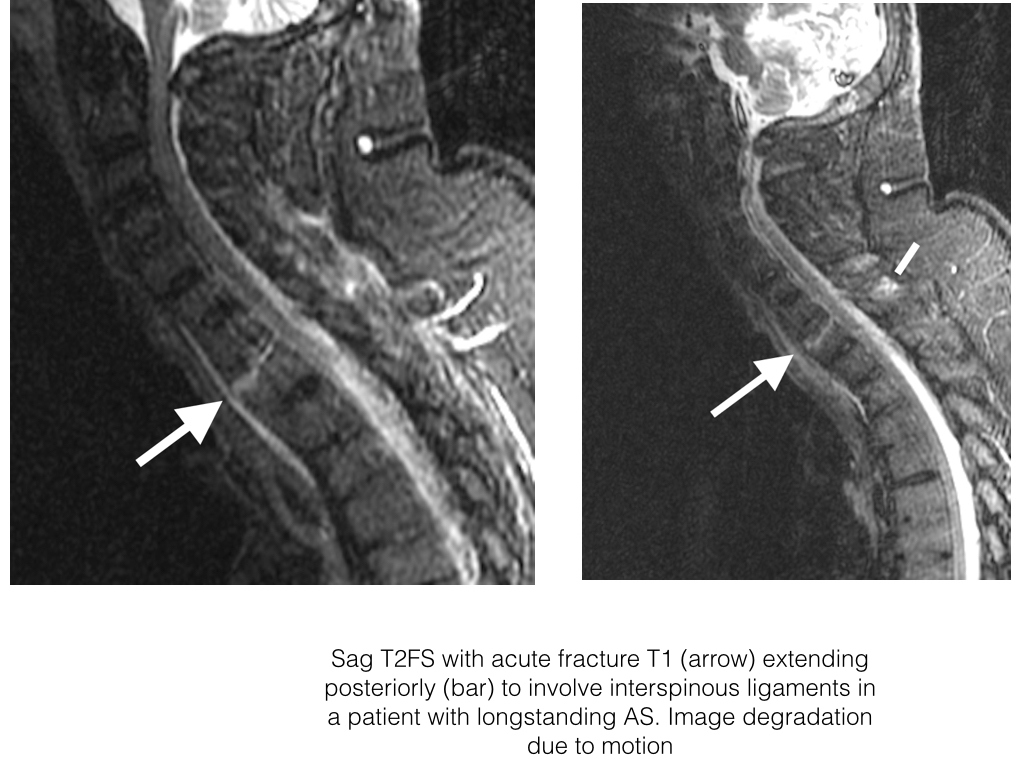
- The diffuse or generalized involves the whole discovertebral junction and can be subdivided into those with and without fractured posterior elements.
- It is a non-infected heterogeneous entity that has two major etiologies, inflammatory and traumatic.
- Localised lesions occur more commonly in the non-ankylosed spine and may relate to inflammation, secondary osteoporosis and herniation of the disc contents through the weakened endplate.
- Radiographs demonstrate localised destruction or erosion of the vertebral endplate with radiolucent foci and surrounding sclerosis.
- MRI demonstrates irregularity to frank erosion of the cortical endplate, adjacent osteitis of increased SI on STIR within the vertebral body, low SI disc and sclerosis deep to osteitis. The posterior elements should be closely evaluated for fracture.
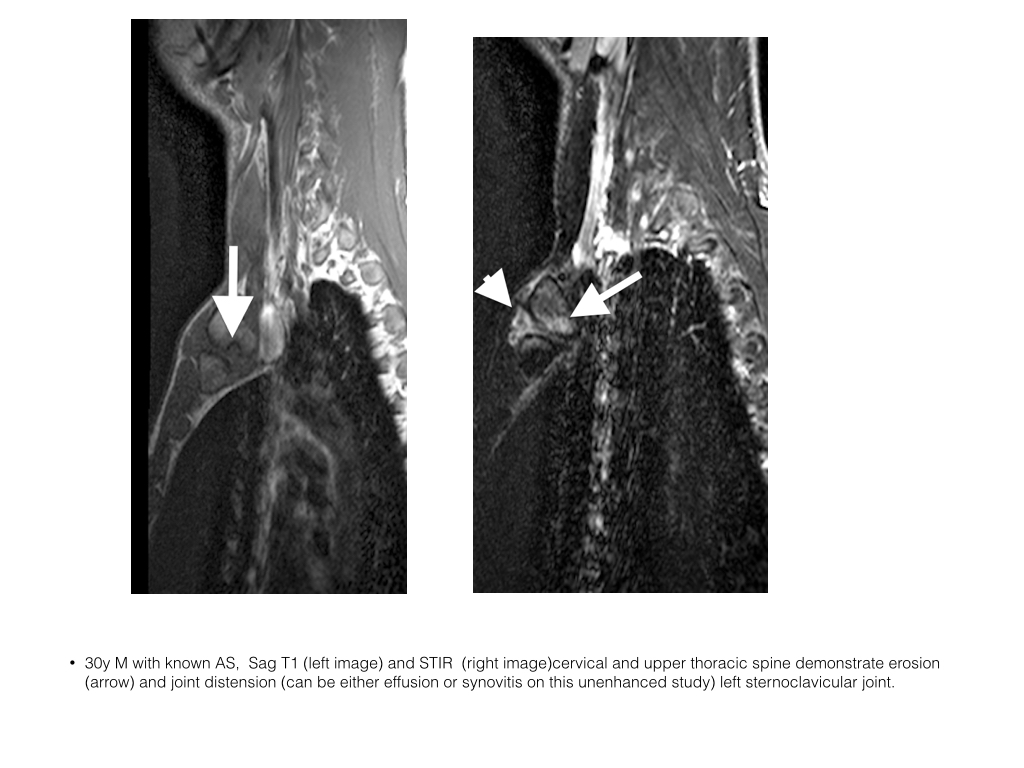
Synovitis
- Synovial tissue lines a synovial joint and is usually not visible on imaging.
- In synovitis the synovium proliferates, is inflamed and edematous and can appear like fluid on MRI i.e. low SI on T1 and high SI on T2FS and STIR.
- Synovitis may occur in the sacroiliac joints, facet joints and sternoclavicular joints on spondylitis imaging
- With intravenous contrast synovium enhances whereas joint effusion does not
- Caveat: post contrast images should be fully acquired not longer than 10 minutes post injection as contrast may diffuse into a joint effusion and hence simulate a synovitis
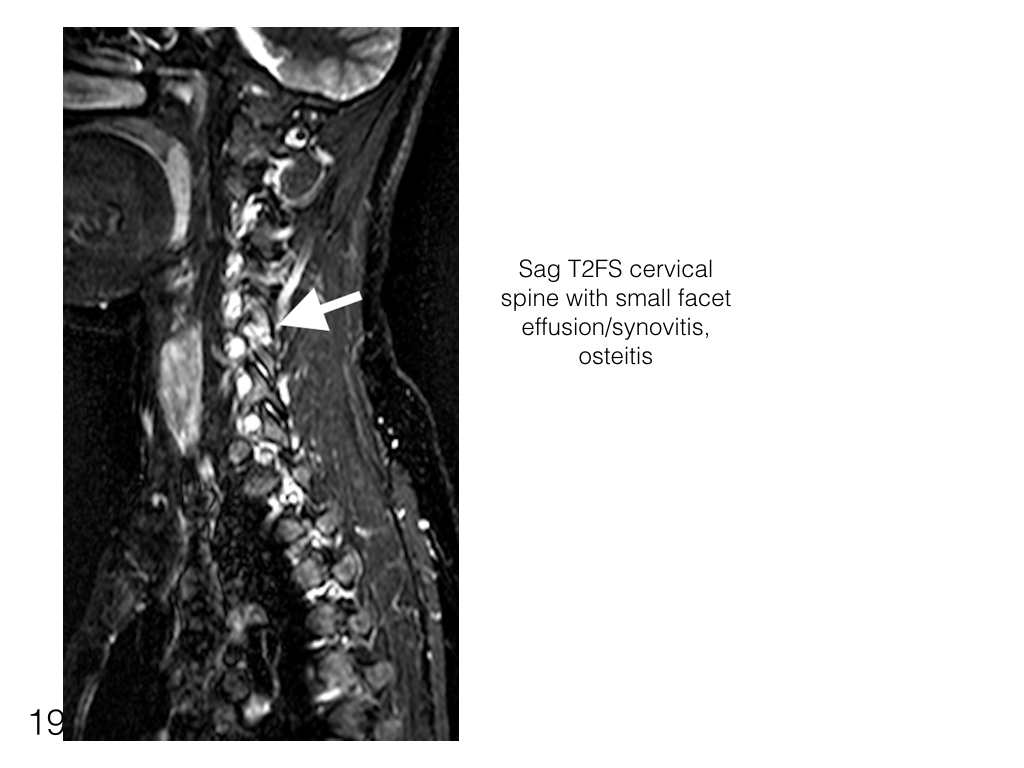
Capsulitis
- Refers to the inflammation of the capsule, a fibrous coating surrounding a joint or organ
- Capsulitis is the acute inflammation of the joint capsule and is only identifiable on MRI.
- Capsular high signal intensity is noted on STIR or contrast enhanced T1FS.
- May extend medially or laterally into the periosteum as an enthesitis
- Occurs in the sacroiliac joints (usually best seen along superior capsule) and the facet joints.
- Often seen in conjunction with other acute inflammatory changes
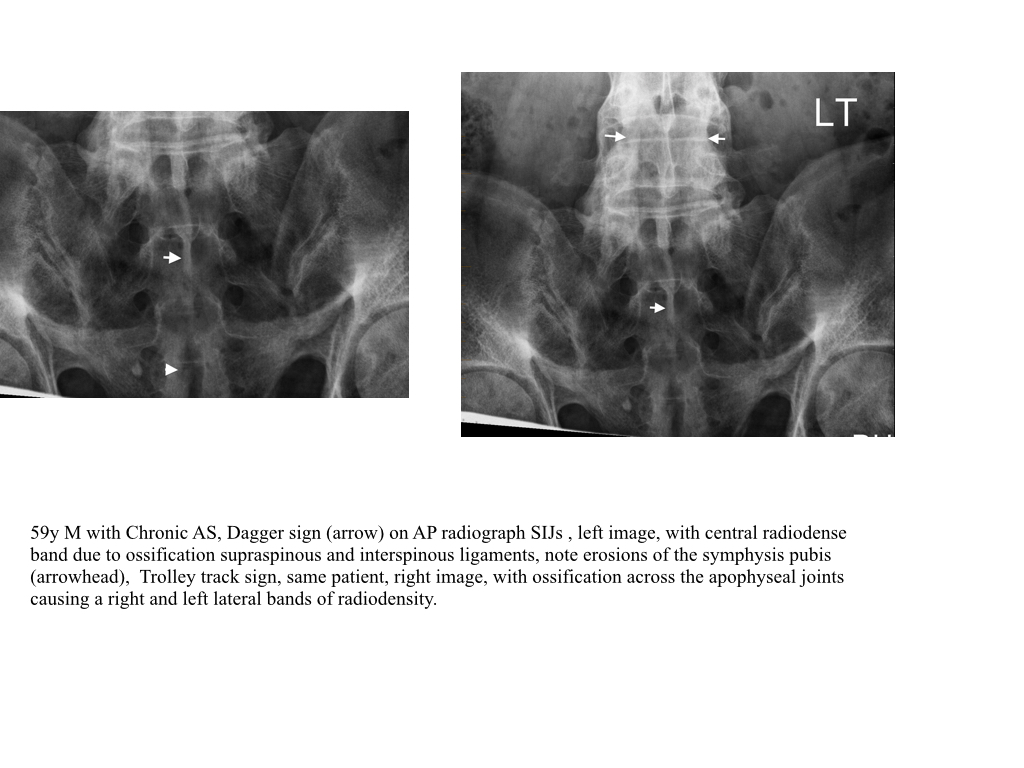
Ligamentous Ossification
- Ligamentous ossification is common in chronic disease.
- The dagger sign, a linear band of radiodensity, white band, on frontal radiograph, is secondary to ossification of the supraspinous and interspinous ligaments.
- When there is additional apophyseal capsule ossification a trolley track sign can be seen on frontal radiographs as three bands of radiodensity superimposed over the spine.
- These changes are usually more evident within the lumbar region.
Osteoporosis
- Osteoporosis is common in longstanding AS
- Discal calcification occurs in chronic disease and may appear ballooned with disc endplate convexity. This is likely secondary to osteoporosis, common in chronic disease.
- BMD assessment of the spine may be inaccurate due to paravertebral ossification as described above and thus lateral spinal assessment is more accurate than AP.
 info_outline
info_outline
Lateral thoracic spine radiograph demonstrating diffuse osteopenia and thinning vertebral cortex. No compression fractures. Note incidental syndesmophytes
Non-Spinal Axial Disease
- Assessment of the sternoclavicular joints and manubriosternal articulation are also often possible when assessing the upper spine.
- Active disease includes osteitis, joint effusion and capsulitis sternoclavicular joint and osteitis at the manubriosternal articulation
- Chronic changes include fusion manubriosternal articulation and erosions at the sternoclavicular joint
Ankylosis
- On radiographs joint space is lost, the subchondral bone plate becomes indistinct and is eventually lost and bone trabecular can be seen transversing the previous joint space.
- CT is excellent in demonstrating bone detail and ankylosis.
- MRI demonstrates continuation of bone marrow signal intensity across the previous joint space.
- Ankylosis occurs most commonly at the SIJs in SpA.
- In the spine the facet joints may become fused.
- In addition ligaments may ossify e.g. the supraspinous and interspinous ligaments (dagger sign on x-ray) and there may be apophyseal capsule ossification (trolley track sign)
Post Inflammatory Fat Accentuation
- PIFA is identified as periarticular high signal intensity on T1 and low signal intensity T1FS and STIR (both have fat suppression).
- Normal bone marrow signal intensity is assessed at the level of the sacral neural foramina and serves as a reference when assessing the periarticular region.
- When the acute osteitis resolves in the spine, the same process occurs as in the SIJs and normal hemopoeitic tissue within the marrow is no longer present and the marrow is predominantly of fat signal intensity.
- These post inflammatory fat accentuation foci (PIFA) appear as high SI on both T1 and T2 sequences and low on T2FS and STIR.
- Commonly seen at the corners of the vertebrae