Sacroiliac Anatomy
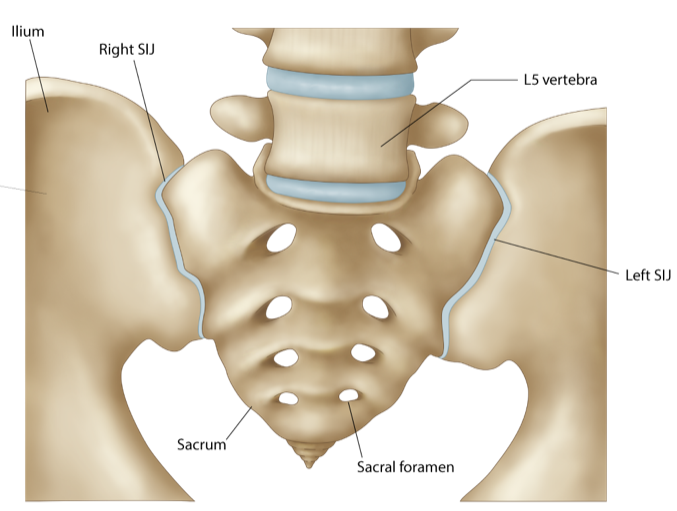
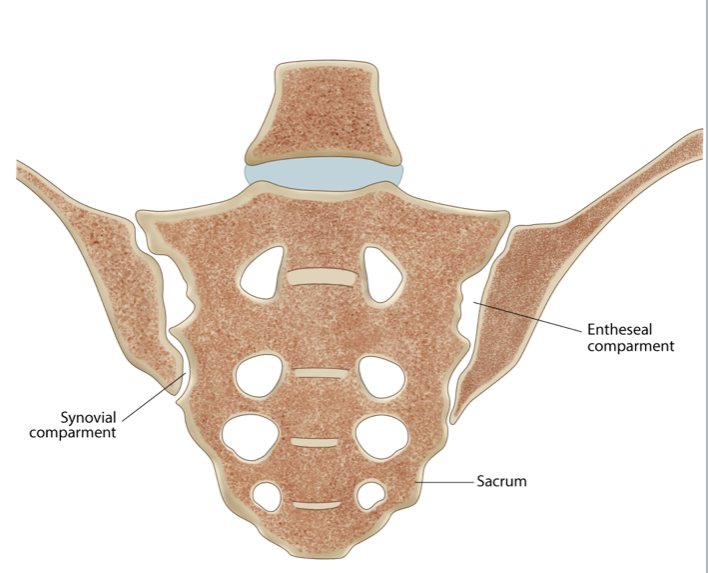
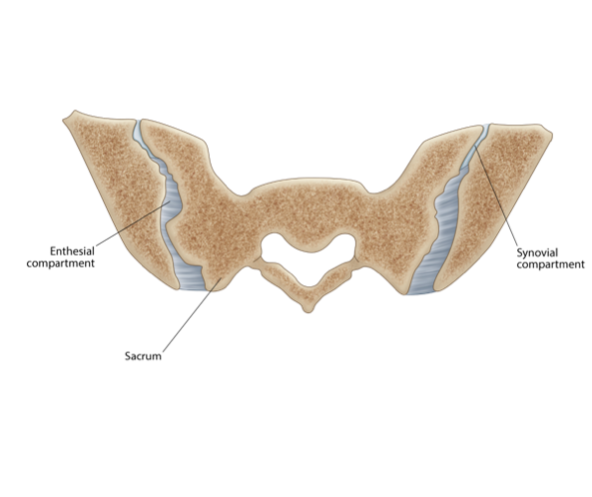
- Traditionally, the SIJs were considered to consist of a smaller posterosuperior ligamentous compartment and a larger anteroinferior synovial compartment.
- More recent research has stimulated a debate on whether the articulation is best classified as a symphysis rather than a synovial joint.
- The articular margins of the sacrum and iliac bones are irregular with interdigitations, which limit mobility and enhance the strength of these joints.
- The articular surface of the sacrum is C or L-shaped, opening dorsally. There are irregular bony pits, dorsal to the articular surface, at the site of ligamentous attachment, the dorsal syndesmosis.
- The articular surface at the centre of the SIJs has hyaline cartilage with fibrocartilage only at the periphery.
- The periphery of the cartilage, with the exception of the distal third of the iliac cartilage, blends with the stabilizing ligaments as in a symphysis and forms a wide margin of fibrocartilage.
- A small synovial recess exists at the ventral aspect of the distal third of the iliac aspect of the joint.
- The SIJ’s are probably therefore best described as a symphysis with characteristics of a synovial joint being restricted to the ventral aspect of the distal cartilaginous portion at the iliac side.
- Under the age of 30 years, the SIJ’s are usually symmetric in appearance.
- A higher prevalence of asymmetric non-uniform joint space narrowing and ill-defined subchondral sclerosis has been observed in women, obese and multiparous females than in age matched males, and individuals of normal weight and non-multiparous respectively.
- The width of the normal SIJ varies from 2 to 5mm.
- The normal SIJ can demonstrate considerable variability, particularly with increasing age.
- Prominent sacral irregularities and marrow defects at the attachment of the interosseous ligaments, termed insertion pits, may be seen in normal subjects.
- Multiple anatomical variants have been observed in patients undergoing pelvic CT for indications other than disease of the SIJ’s. These include:
- Accessory joints (19)
- Bipartite iliac bony plate (4)
- Semicircular defects at the sacral or iliac side (3)
 info_outline
info_outline
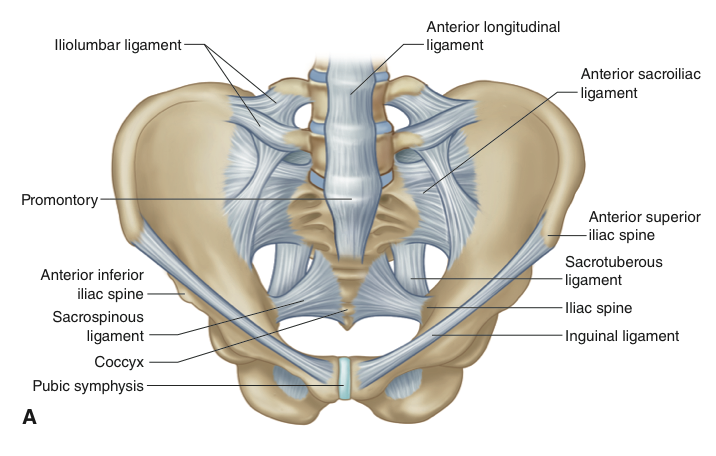
a) Illustration normal anatomy of the sacroiliac joints with overlying ligaments-Anterior view
 info_outline
info_outline
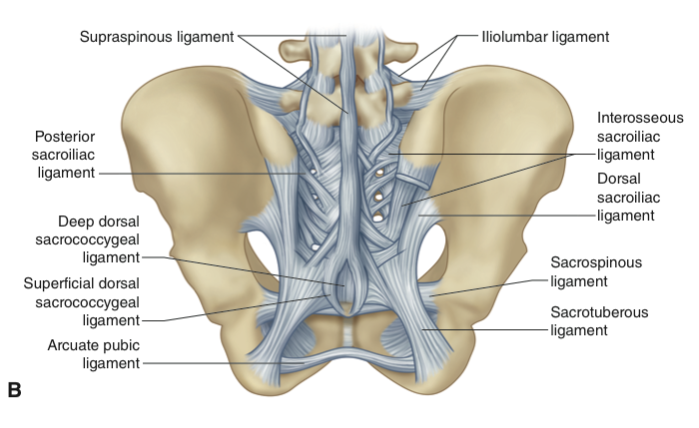
b) Illustration normal anatomy of the sacroiliac joints with overlying ligaments-Posterior view
 info_outline
info_outline
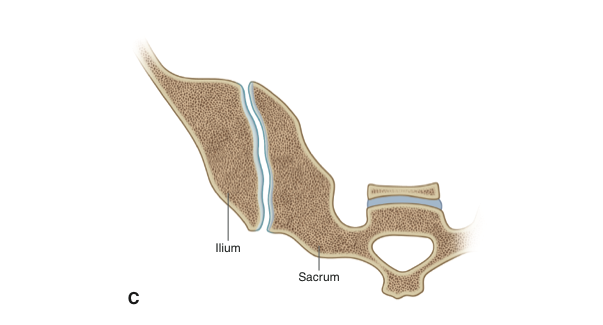
c) Illustration normal anatomy of the right sacroiliac joint -axial cut through the joint demonstrating normal interdigitations of the articulation
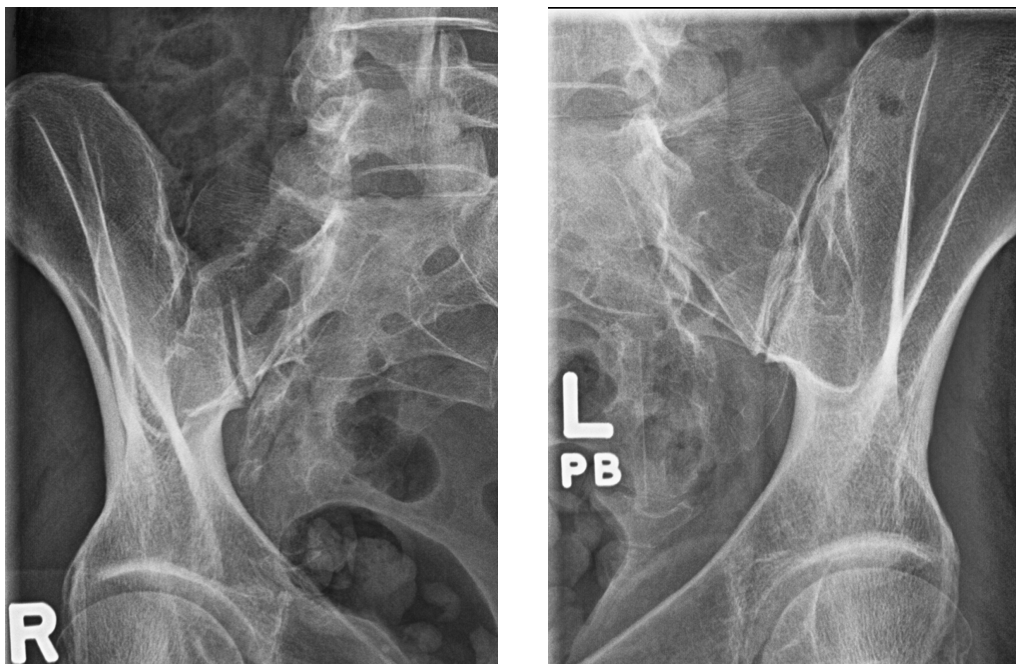
Sacroiliac Radiograph
- Plain radiography has and continues to play an important role in the investigation of SII and is an integral part in the diagnosis of AS.
- The anatomy of the sacroiliac joint, due to its oblique nature and overlap of the sacral and iliac components, has led to significant inter and intra observer variations particularly in the interpretation of early SII.
- Radiographic projections include dedicated AP and bilateral oblique views. If the AP study is normal then the oblique views may not be required
- Note that a dedicated AP of the lumbar spine often includes a diagnostic assessment of the SIJ and may not require any further radiographs.
- Radiographs of the lumbar spine and SIJ incur a significant radiation dose (Single AP lumbar spine has a typical effective dose of up to 0.7mSV)
- Some centres advocate a baseline AP of the pelvis. This allows for a combined assessment of the sacroiliac joints and the hip joints, the latter may be involved in up to 25% of patients with SpA.
 info_outline
info_outline
AP Normal Sacroiliac Joints
 info_outline
info_outline
Illustration Normal Sacroiliac Joints
 info_outline
info_outline
Right & Left Oblique Radiographs SIJ
Sacroiliac MRI
- MRI is the imaging gold standard for sacroiliitis.
- MRI is non-ionizing, provides excellent anatomical detail and delineation of both acute and chronic changes of sacroiliitis.
- We will briefly review the anatomy of the sacroiliac joints on MRI prior to reviewing pathological changes.
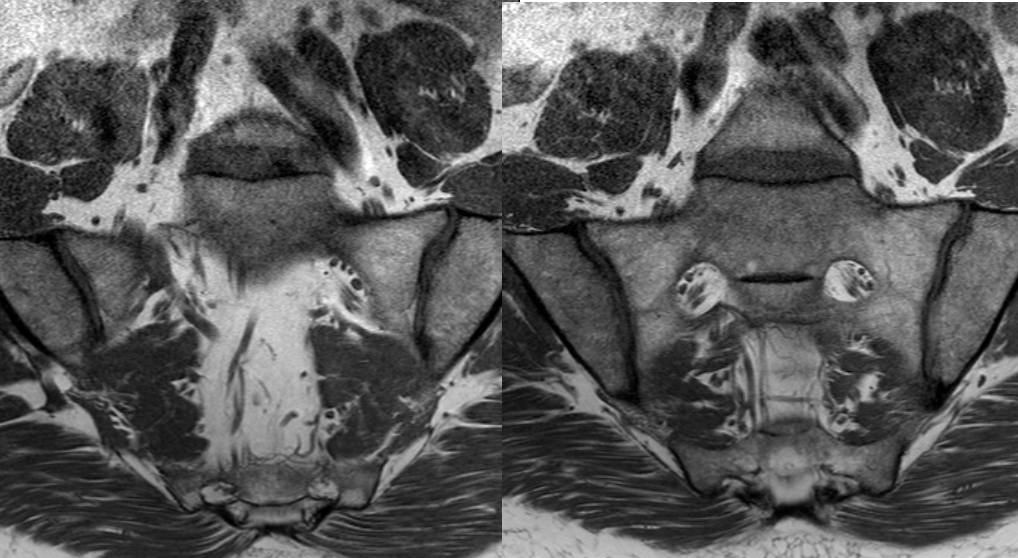
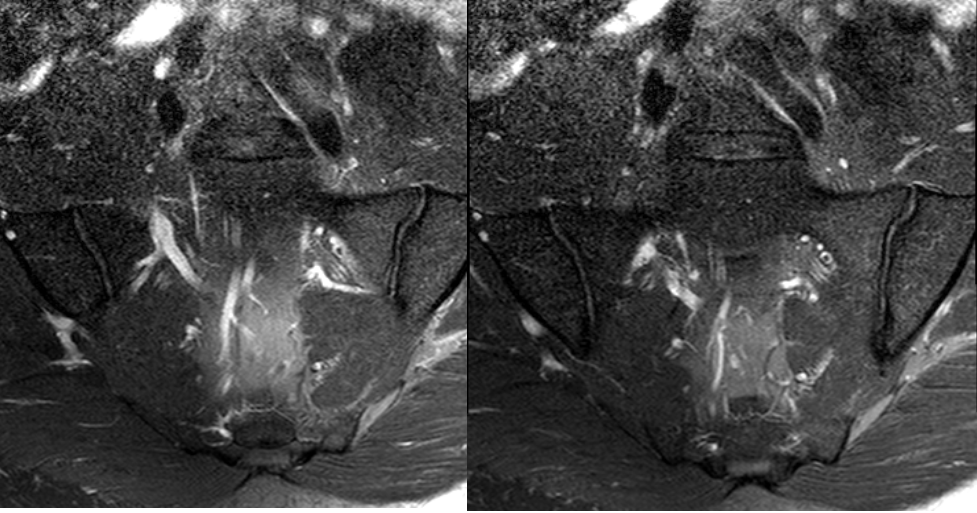
Coronal T1 SIJ (from anterior to posterior)
- Standard semicoronal T1 sequence (without fat saturation) is excellent in assessing the normal anatomy of the SIJs.
- The joint space is low signal intensity (SI), articular cartilage is low to intermediate and is not optimally assessed.
- The subchondral bone plate is seen as a thin linear uninterrupted low SI line deep to the cartilage.
- Deep to the subchondral bone plate is the subchondral bone marrow which can vary in SI depending on the age of the patient, in younger patients there is more abundant red marrow which is of intermediate SI and slightly higher than muscle which is replaced by increasingly fatty marrow as one ages and becomes higher in SI. The normal subchondral marrow should be of similar SI to the sacral marrow at the level of the sacral foramina.
 info_outline
info_outline
a) Coronal T1 SIJ (from anterior to posterior)
 info_outline
info_outline
b) Coronal T1 SIJ (from anterior to posterior)
 info_outline
info_outline
c) Coronal T1 SIJ (from anterior to posterior)
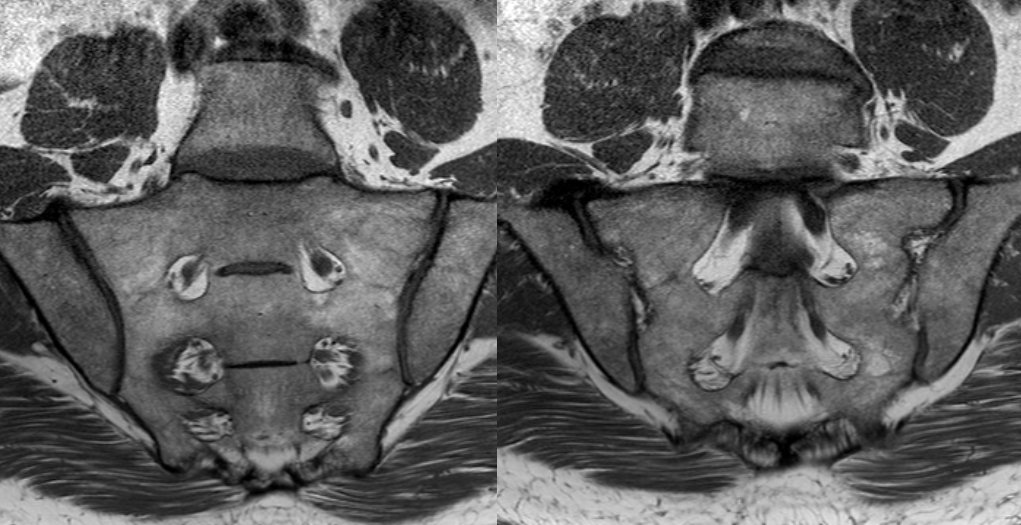
Coronal T2FS SIJ (from anterior to posterior)
- T1FS (T1 Fat Saturated) is not commonly performed in the standard evaluation of the SIJs. It is more sensitive in the visualization of the articular cartilage, intermediate to high signal intensity, and adjacent subchondral bone and thus more sensitive than standard T1 in the assessment of erosions. Because marrow fat is suppressed in this sequence it is less useful in the assessment of the subchondral marrow, hence why it is not routinely used.
- Subchondral bone plate is thin, regular and of low signal intensity
- The subchondral marrow is low signal intensity, due to the suppression of the normal fat signal within normal marrow.
 info_outline
info_outline
a) Coronal T2FS SIJ (from anterior to posterior)
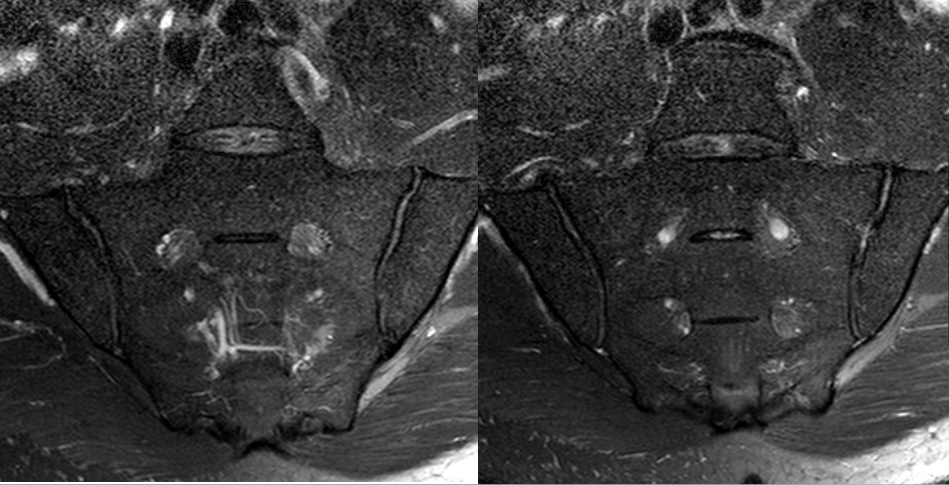 info_outline
info_outline
b)Coronal T2FS SIJ (from anterior to posterior)
 info_outline
info_outline
c) Coronal T2FS SIJ (from anterior to posterior)
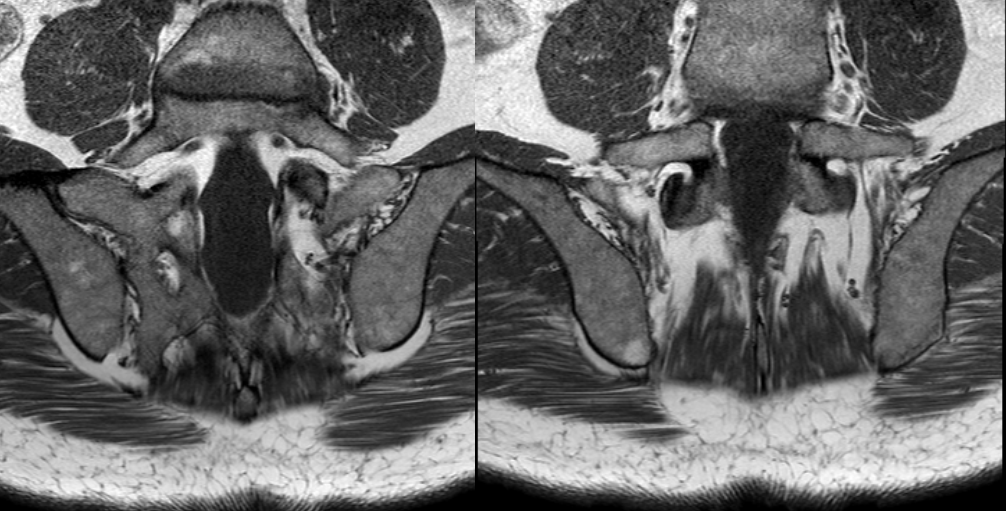
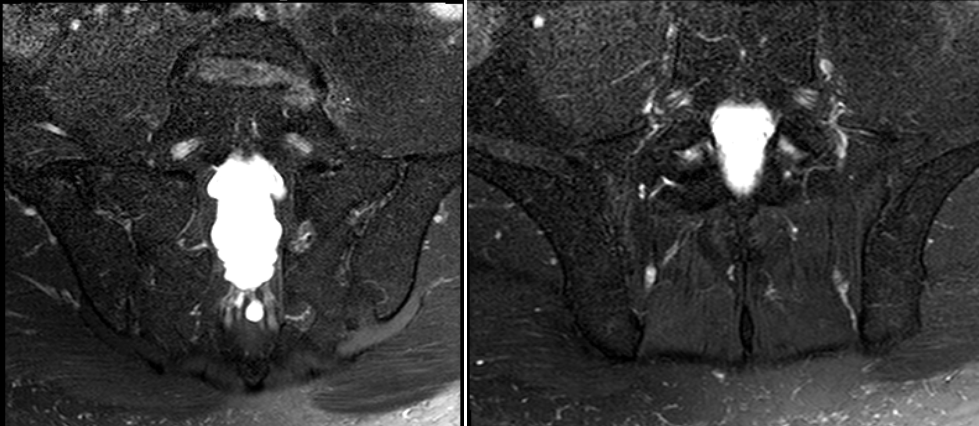
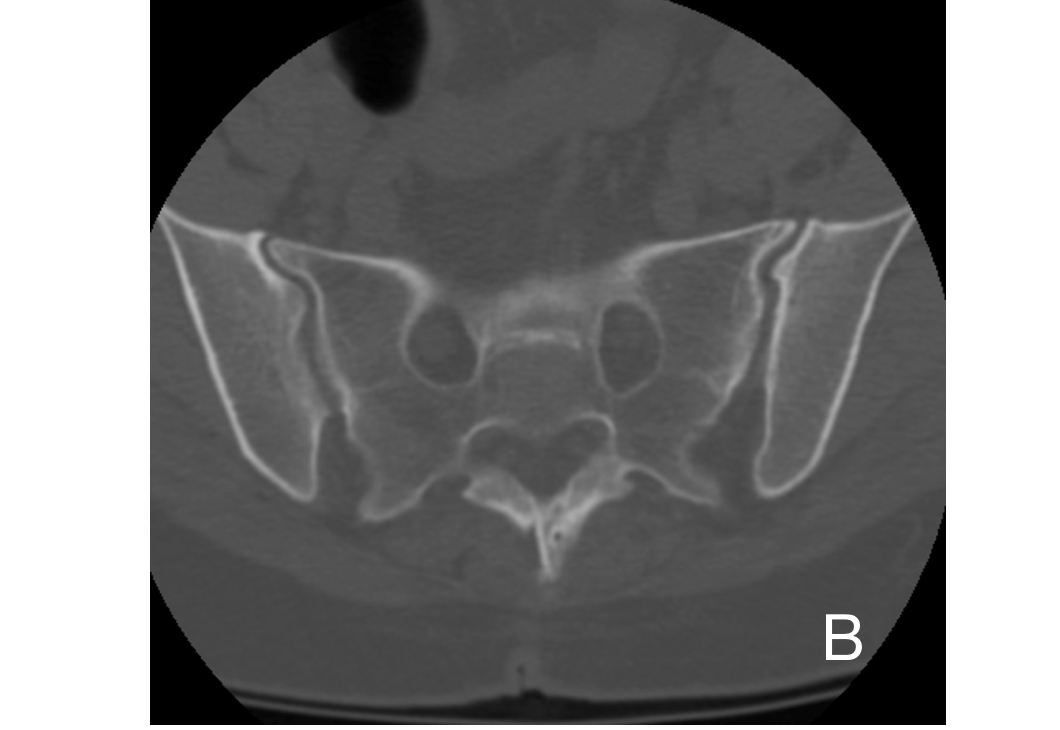
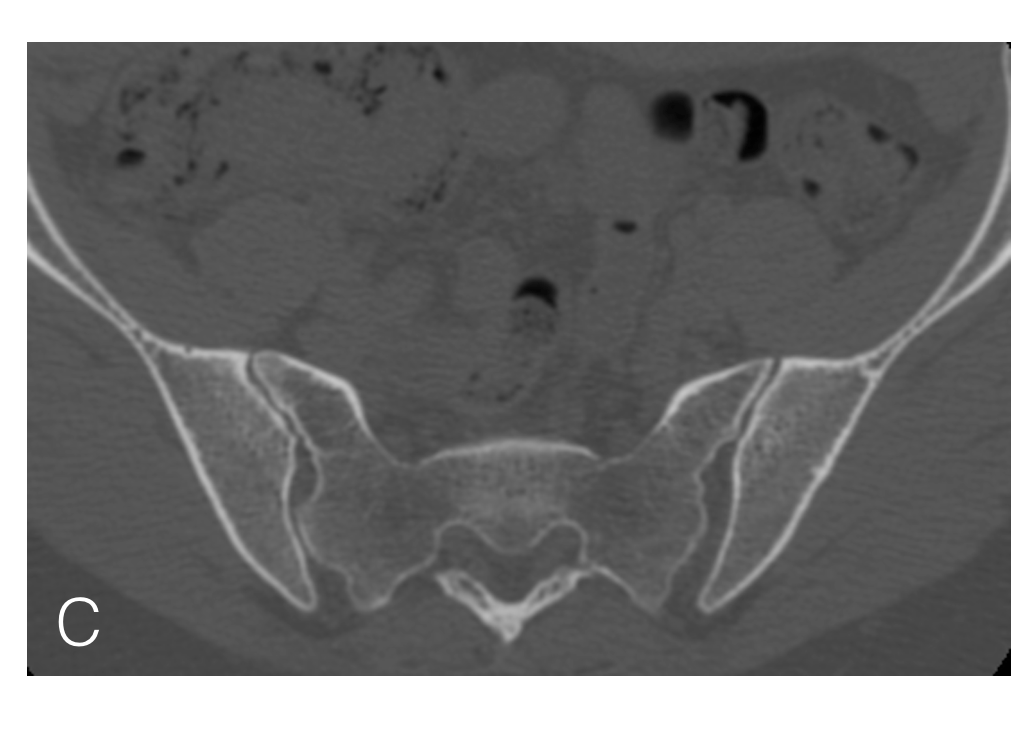
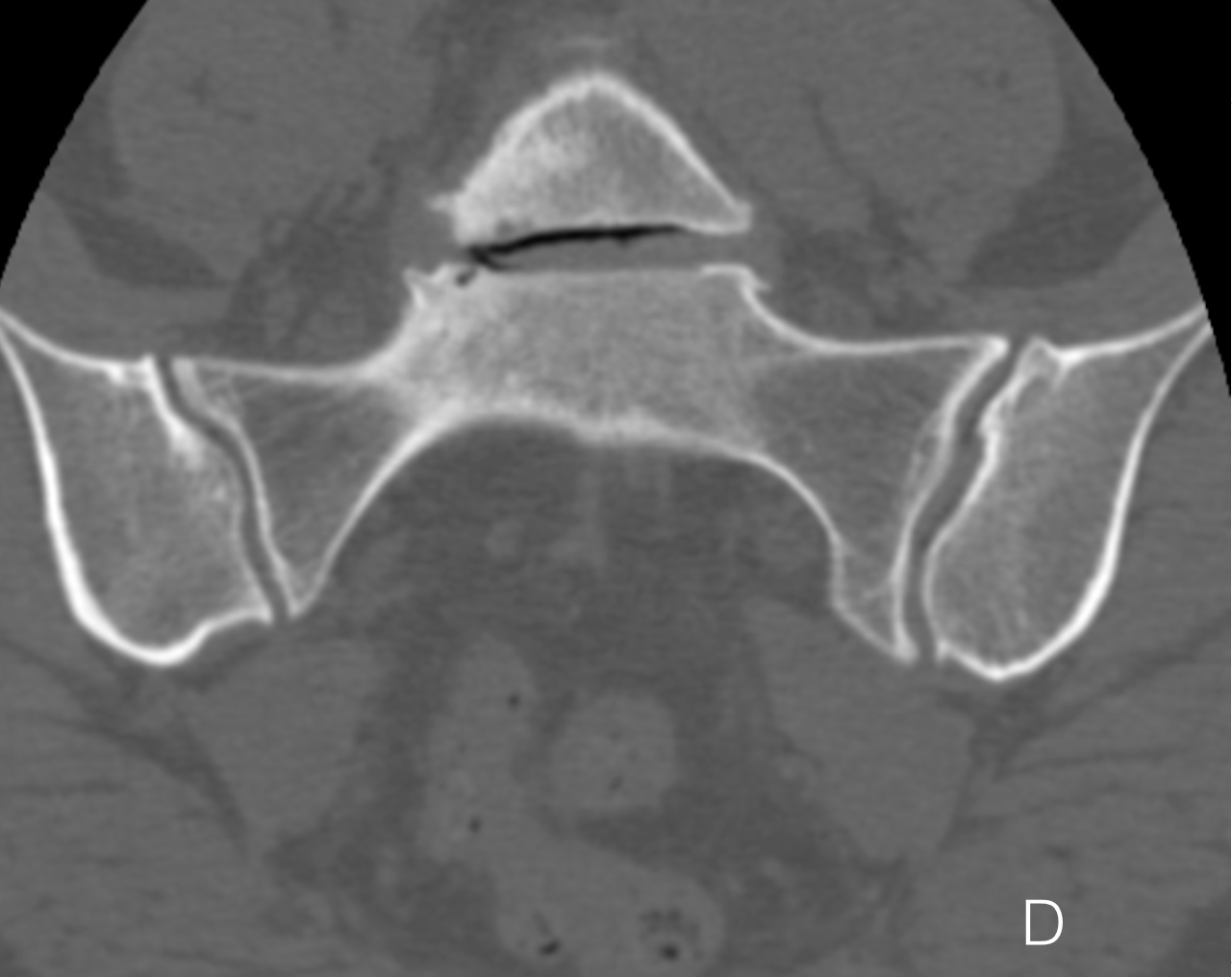
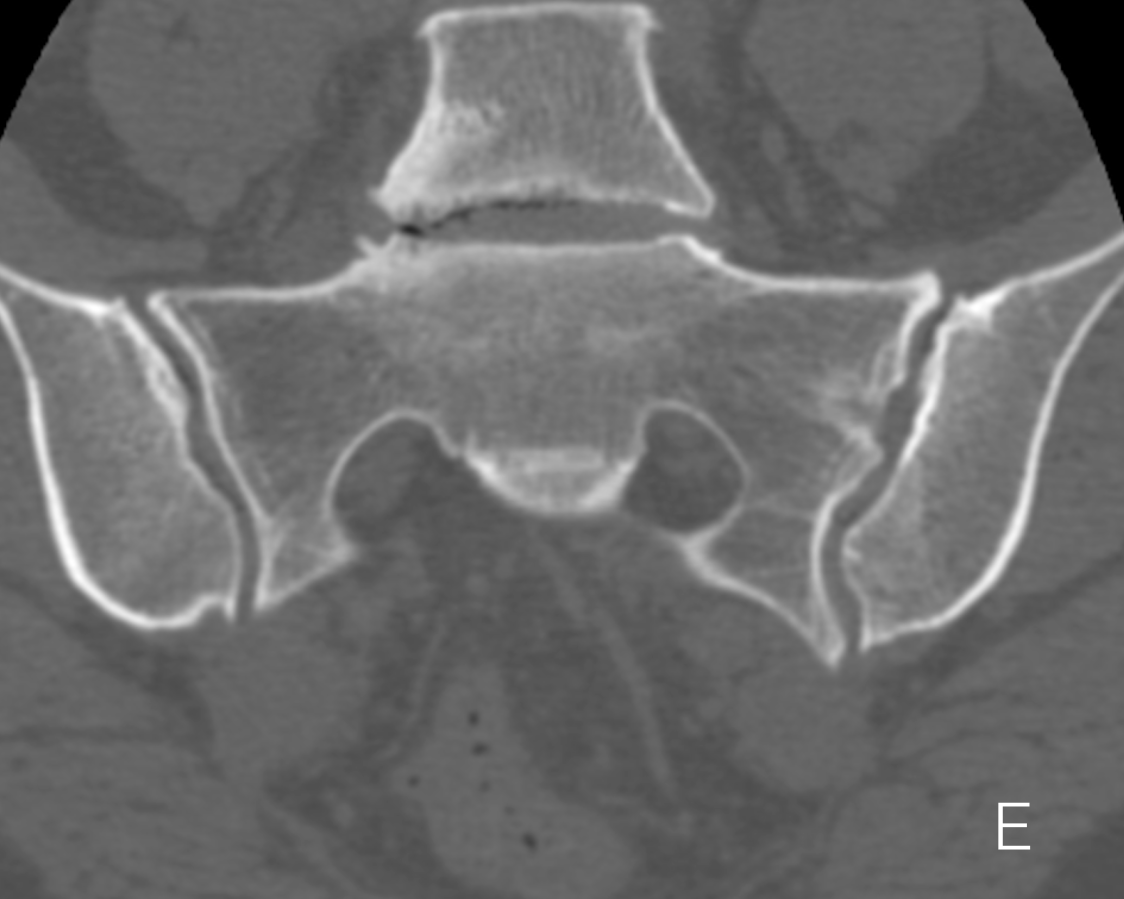
Sacroiliac CT
- CT provides excellent bone detail and is the gold standard in the assessment of erosions.
- The joint space, subchondral bone plate, subchondral bone are clearly delineated.
- CT can not detect bone marrow Edema and has low sensitivity for post inflammatory fat accentuation and joint effusions
- CT incurs a significant radiation exposure and imaging is usually confined to those patients who are unable to undergo MRI and diagnosis/management options can not be satisfied with radiographs
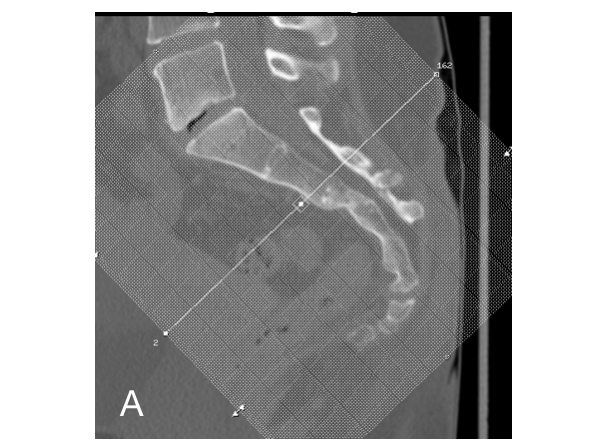
Semicoronal CT Sacroiliac Joints
A) localiser image sacrum, the scan planes are acquired from this image, the line transversing the image is in the true axial plane sacrum as demonstrated in b) & c), d) and e) are true coronal through the sacroiliac joints and f) is a sagittal reconstruction (usually not required for sacroiliac disease but may be beneficial for other pathology including fracture assessment)
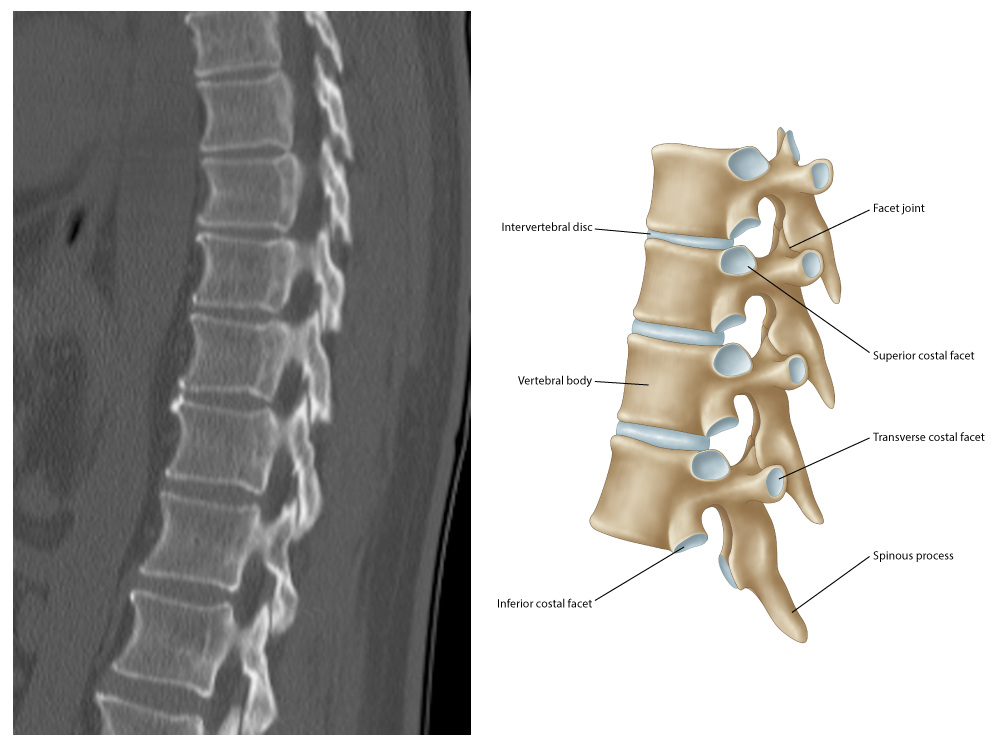
Spinal Anatomy
- The vertebral column extends from the skull base to the inferior coccyx and is composed of 33 vertebrae: 7 cervical, 12 thoracic, 5 lumbar, 5 fused sacral vertebrae forming the sacrum, and 4 coccygeal vertebrae.
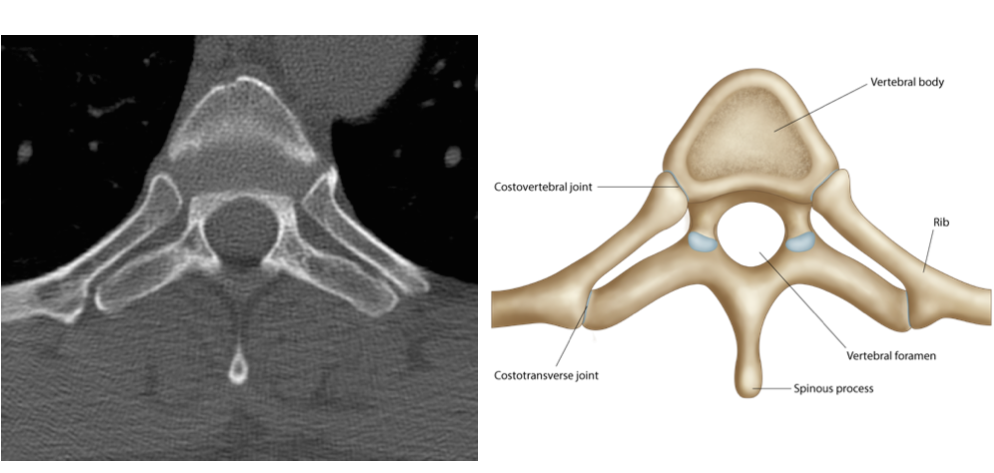
- A typical vertebra is composed of a body anteriorly and a vertebral arch posteriorly. They enclose the vertebral foramen or spinal canal.
- The latter is composed bilateral pedicles anteriorly and bilateral lamina posteriorly.
- The bilateral transverse processes (projecting laterally) arise from the junction of the pedicles and lamina, and the spinous process from junction lamina (projecting posteriorly)
- There are four articular processes, bilateral superior and inferior, articulating with the vertebra above and below respectively at synovial joints called the facet joints.
- The intervertebral foramen passes between the pedicles of adjacent vertebrae and have small notches to help create the foramen.
- Thoracic vertebrae have costal facets for articulation with head of the ribs. These form the costovertebral joints.
- Similarly the transverse processes of the thoracic vertebrae articulate with the ribs at costotransverse joints.
- Intervertebral disc are composed of an outer annulus fibrosus. This consists of concentric rings of fibrocartilage. The outermost fibres are attached to the anterior and posterior longitudinal ligaments.
- Peripheral fibres enter adjacent vertebral bone, Sharpey’s fibres.
- The nucleus pulposus is contained centrally by the annulus fibrosus. It is gelatinous with a high water content and desiccates as one ages. It serves as a shock absorber.
- In general there are 23 discs: 6 cervical, 12 thoracic and 5 lumbar.
- Discs articulate with adjacent vertebra, which have a thin layer of hyaline cartilage, at a fibrocartilaginous joint.
- Anterior Longitudinal Ligament - attaches to the anterior vertebral body and discs. Extends inferiorly from the atlas to the superior sacrum.
- Posterior longitudinal ligament- firmly attaches to posterior discs and loosely attached to vertebrae. Extends from axis (continued superiorly as tectorial membrane) to the superior sacrum.
- Supraspinous ligament extends between tips of spinous processes (becomes ligamentum nuchae in cervical spine)
- Interspinous ligament runs between adjacent spinous processes
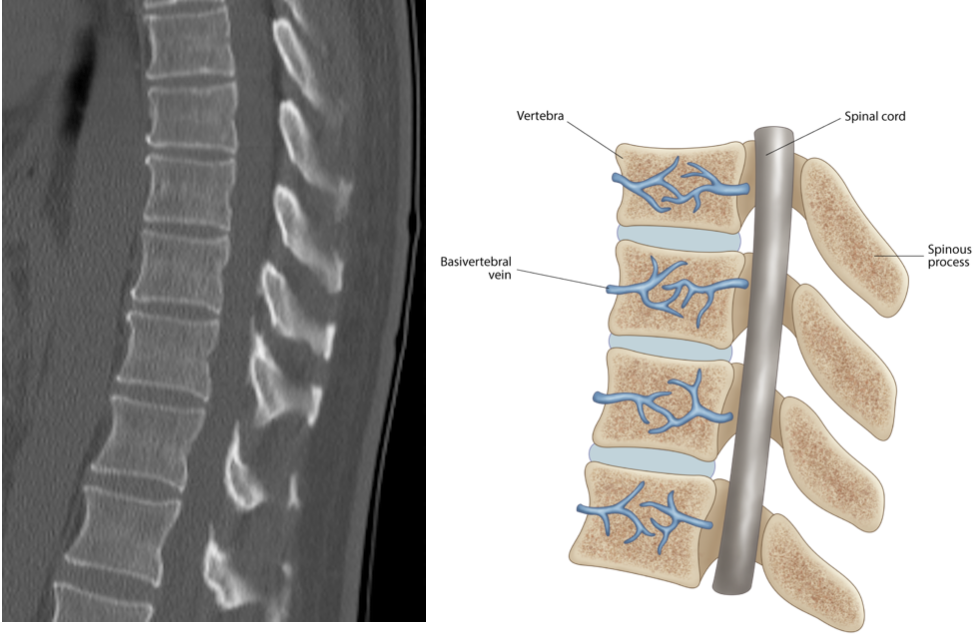 info_outline
info_outline
a) Sagittal CT Mid Thoracic Spine
 info_outline
info_outline
b) ParaSagittal CT Thoracic Spine
 info_outline
info_outline
c) Axial CT Thoracic Spine
Spinal Radiographs
- Note that the AP radiograph of the lumbar spine often allows for assessment of the sacroiliac joints and no further radiographs may be required (cave:radiation exposure)
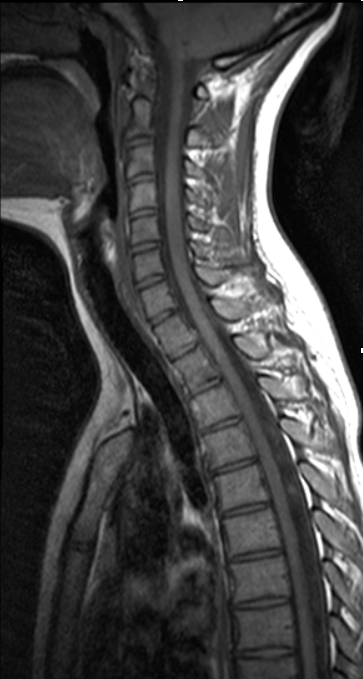
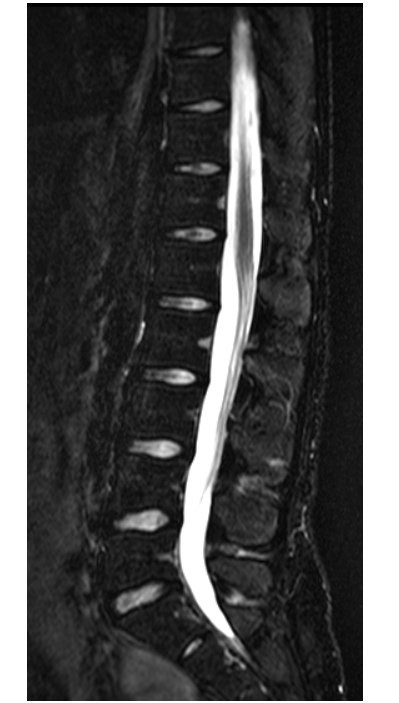
Spinal MRI
- MRI acquisition of the spine includes Sagittal T1 and STIR or T2FS sequences.
- The whole spine is imaged at many centres whereas some centres will image mid-thoracic to the lumbosacral junction.
- Whole spine imaging is divided into 2 separate field of views i.e cervical to mid thoracic spine and mid thoracic to lumbosacral junction. The two images are then overlayed to provide a full spinal image.
- Axial imaging is usually not acquired . Assessment of degenerative disc disease is limited in these studies given the larger field of view and lack of axial imaging
Spinal CT
- CT of the whole spine is not performed for SpA given the extended field of view and subsequent large radiation exposure.
- Occasionally localized regions are acquired if MRI is unavailable e.g. assessment of fractures in patient with SpA.
- Discussion with your radiologist to determine optimal imaging pathway in complex cases is always encouraged.
 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline

 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline