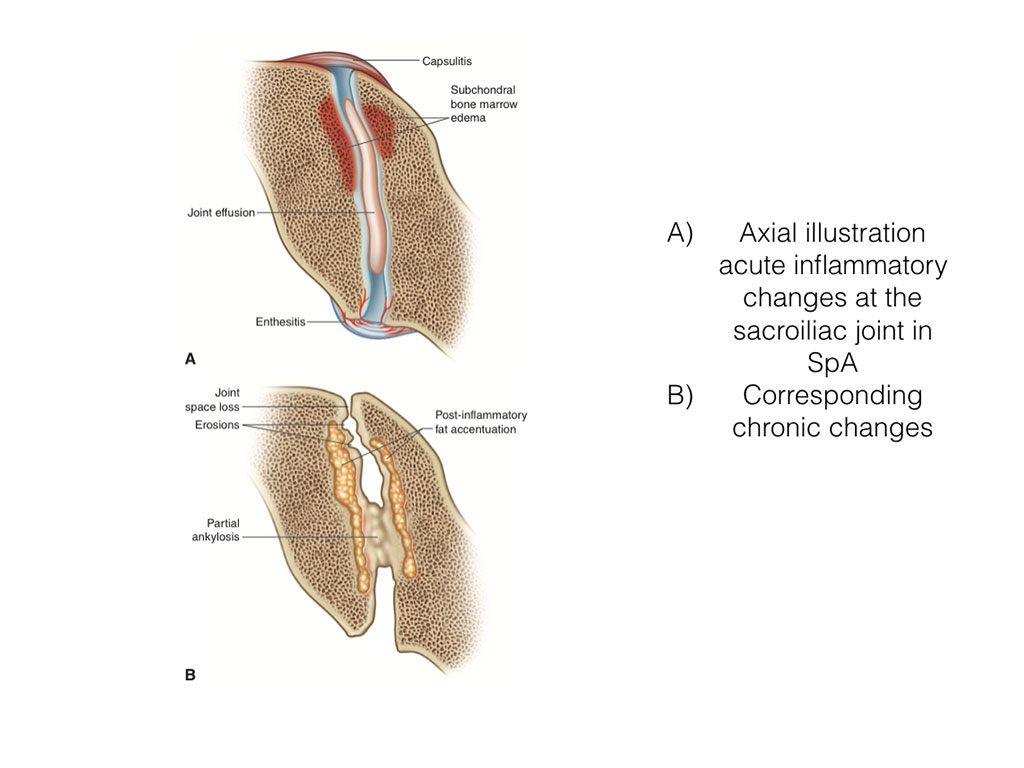
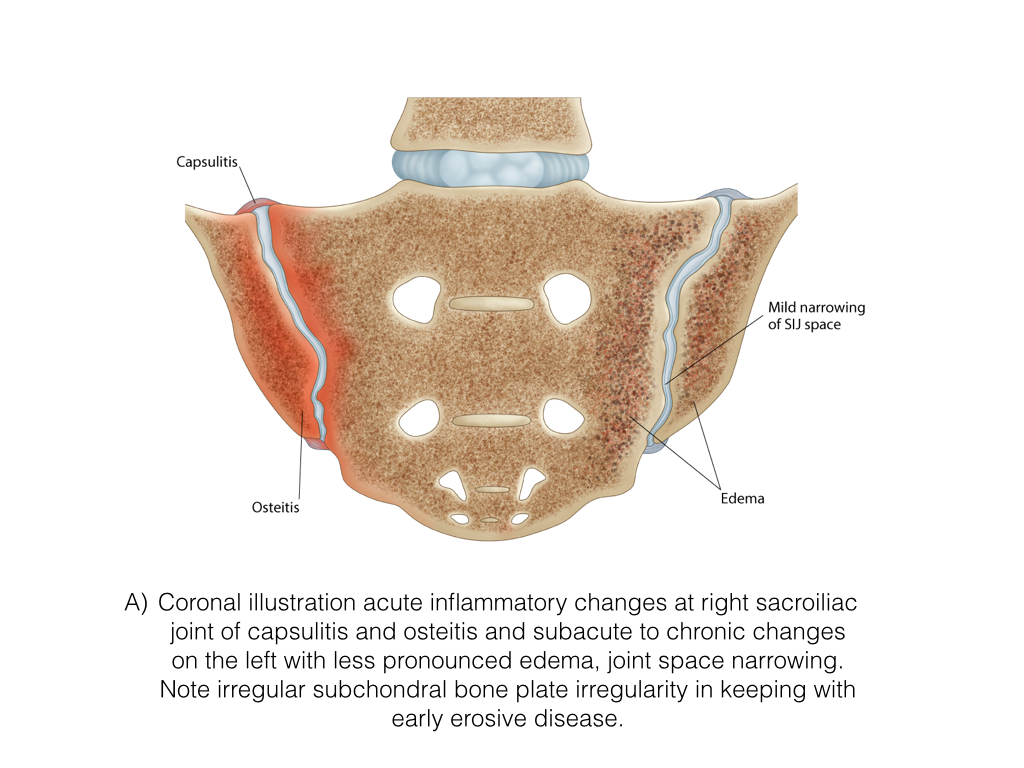
Edema & Osteitis
- Edema is an excess accumulation of fluid in the bodies tissue and can occur from multiple causes.
- With respect to SpA we will focus on edema related to inflammation.In the case of bone this inflammatory changes is called osteitis.
- Enthesitis and capsulitis are related to inflammatory changes and edema at ligament or tendon attachment to bone and joint capsule respectively
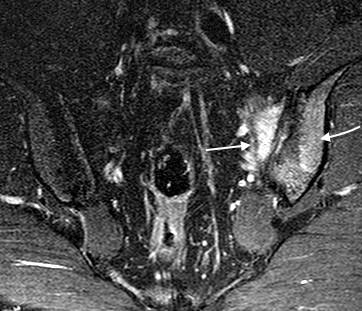
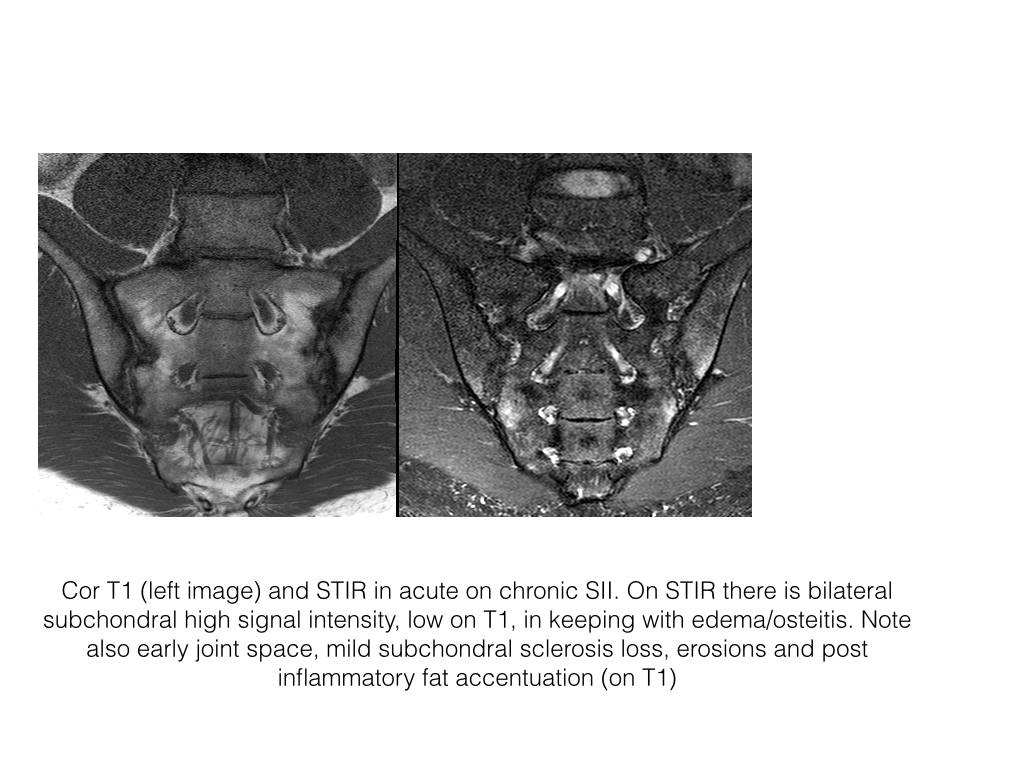
Osteitis-SIJ
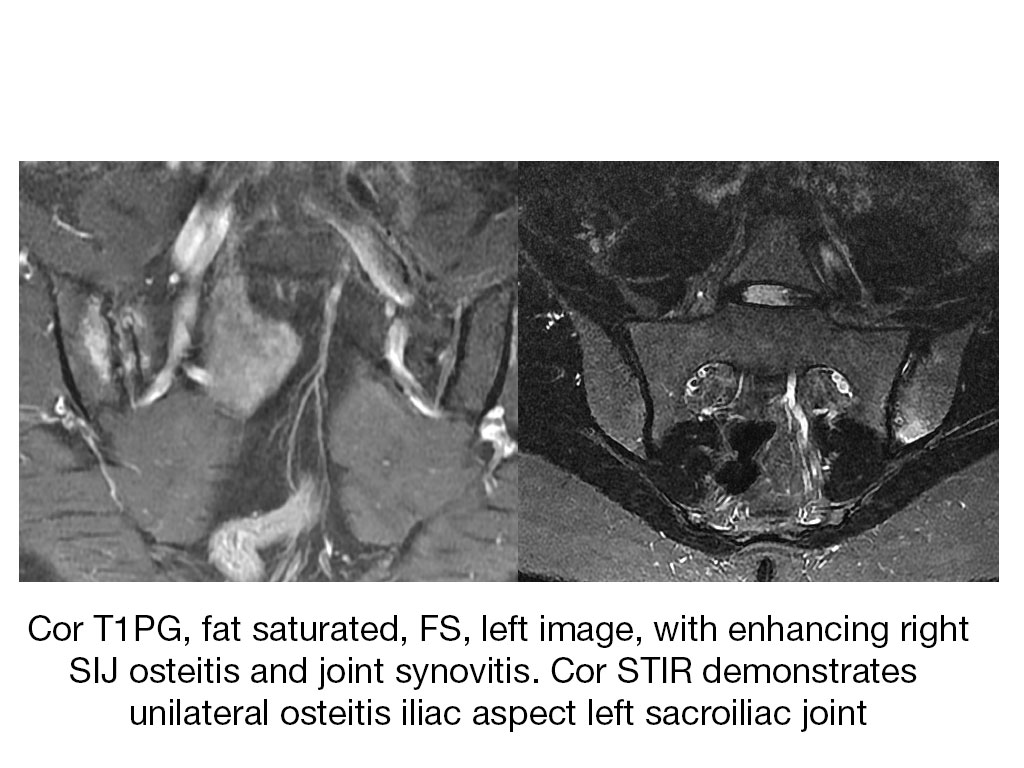
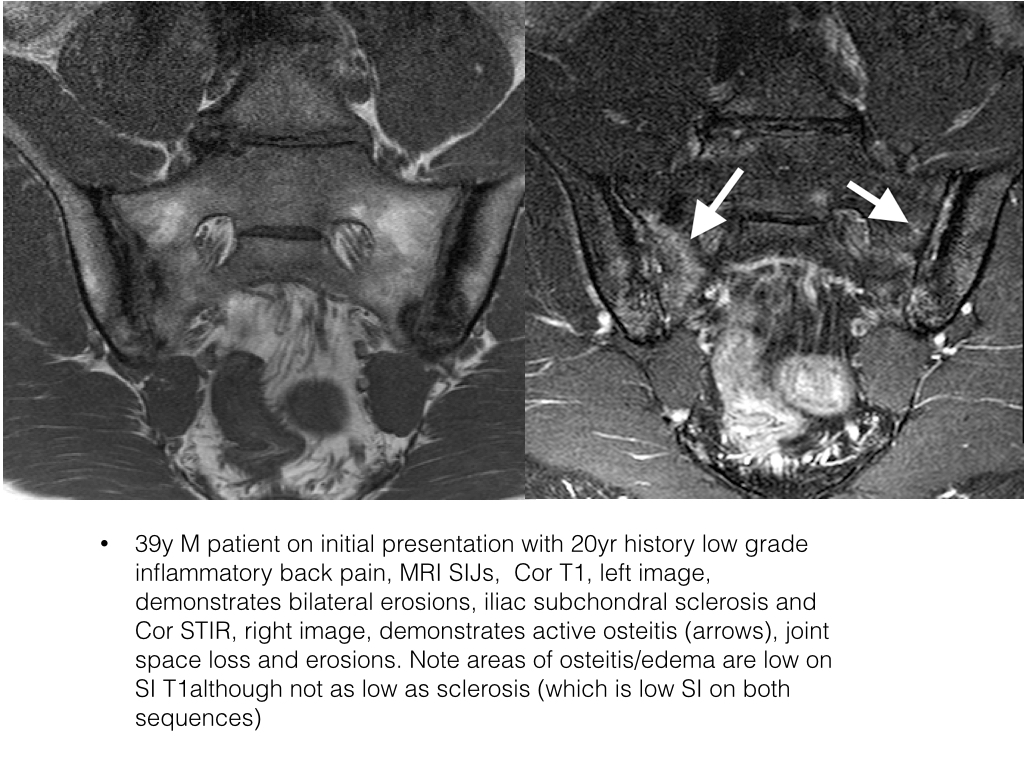
- When depicted in MR imaging, edema presents with periarticular high signal intensity on STIR, T2FS and contrast enhanced T1FS.
- Usually occurs first on the lilac aspect joint, thought to be related in part to thinner cartilage on this side and transversing channels through the subchondral plate
- Osteitis is difficult to appreciate on T2 without fat saturation as edema and marrow signal intensity are similar
- On T1 edema is of intermediate to low signal intensity
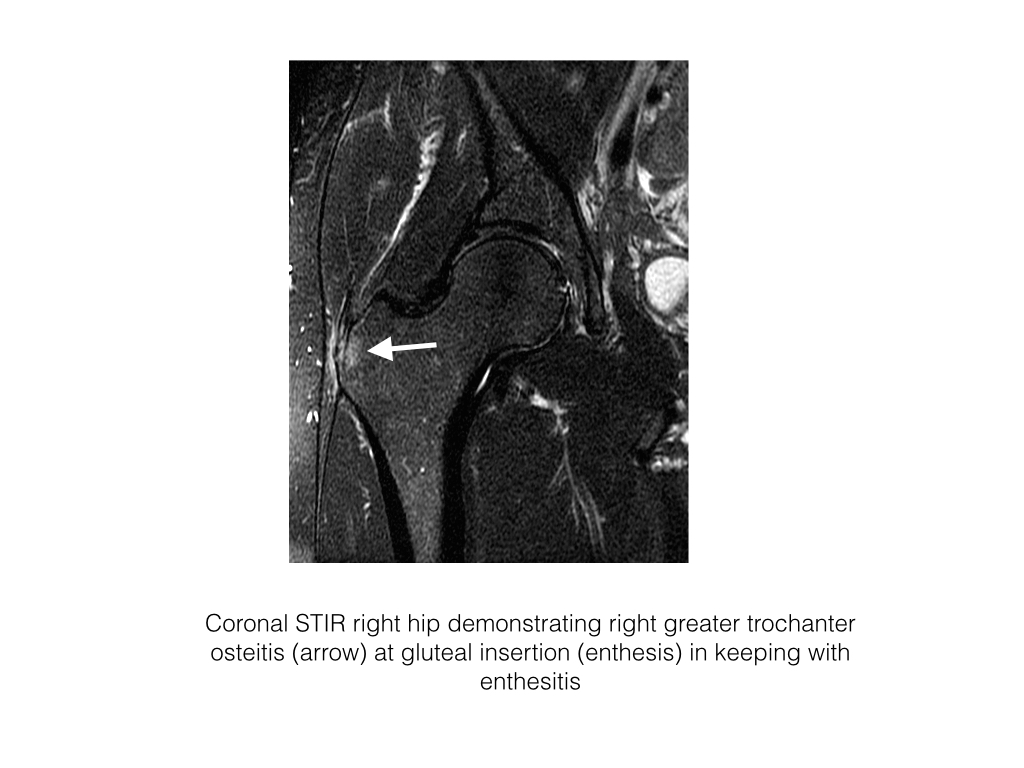
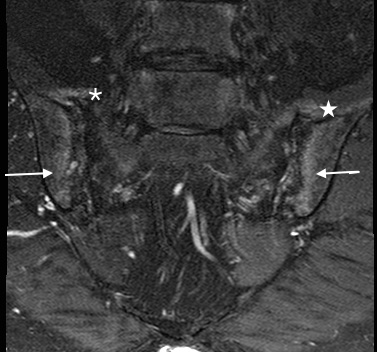
Enthesitis
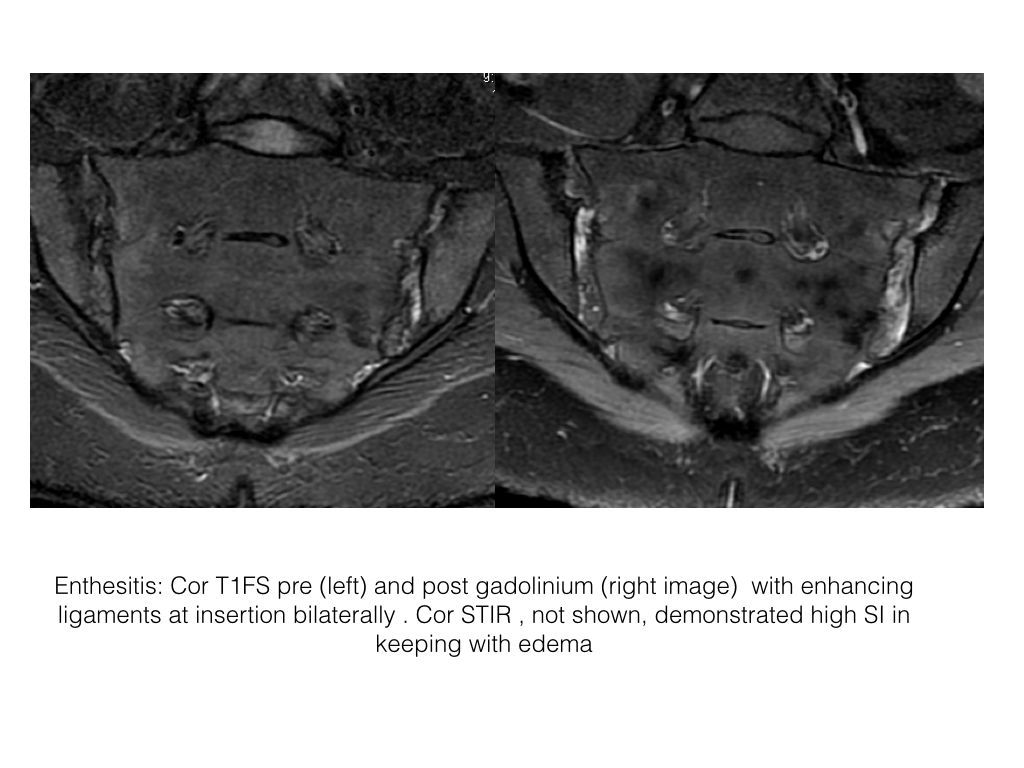
- Enthesitis is the inflammation of the enthesis, site of insertion of tendon, ligament or joint capsule to bone.
- There are 2 types of entheses, fibrous and fibrocartilaginous
- Enthesitis is common in SpA. It may be subclinical and detected only on imaging.
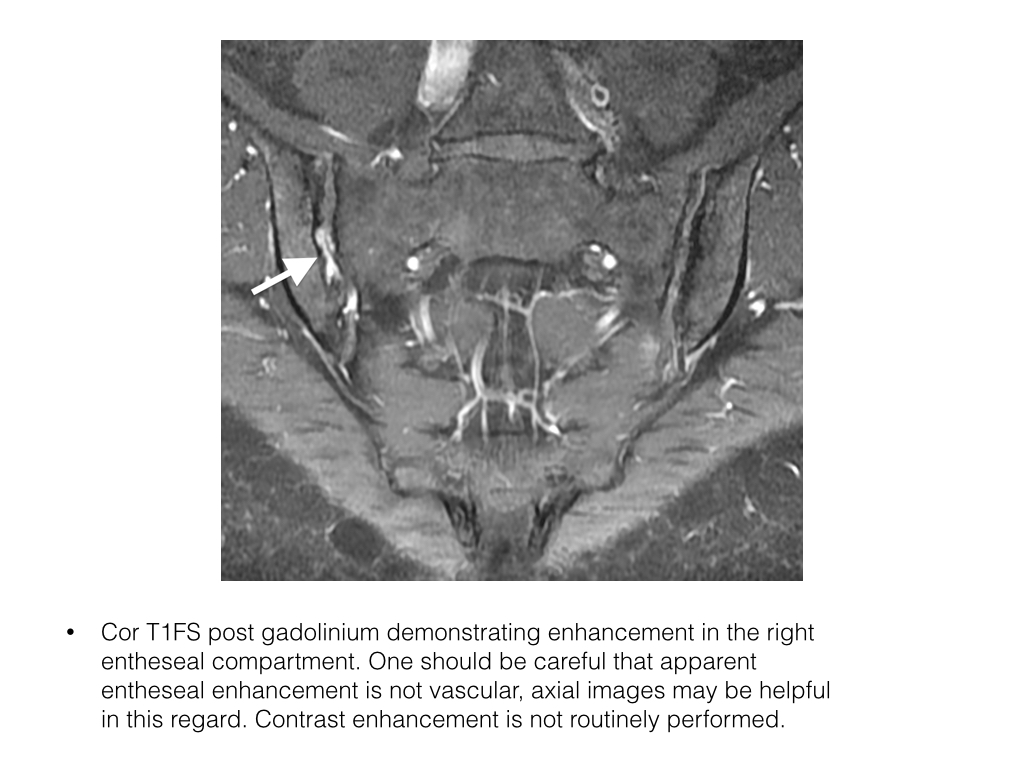
- On MRI enthesitis is identified as high signal intensity on STIR or contrast enhanced T1FS at the site of ligament, tendon or capsular attachment to bone.
- Ultrasound is not used clinically in the assessment of axial enthesitis due to the depth of tissue and the availability of MRI.
- CT can not assess osteitis or enthesitis.
- Nuclear studies with bone scan would demonstrate increase uptake at sites of osteitis but is non-discriminatory, is not as sensitive as MRI and incurs a significant radiation dose.
Enthesitis-SIJ
- With respect to the SIJs it is best visualized in the entheseal compartment, posterior to the cartilaginous joint, posteriorly at gluteal tendon attachment, superiorly and anteriorly at capsular attachment.
Enthesitis-Peripheral
- Peripheral enthesitis can be assessed with ultrasound and demonstrates a thickened heterogenous tendon at insertion with increased internal flow on Doppler. There may be related bursal distension. Ultrasound can not assess osteitis.
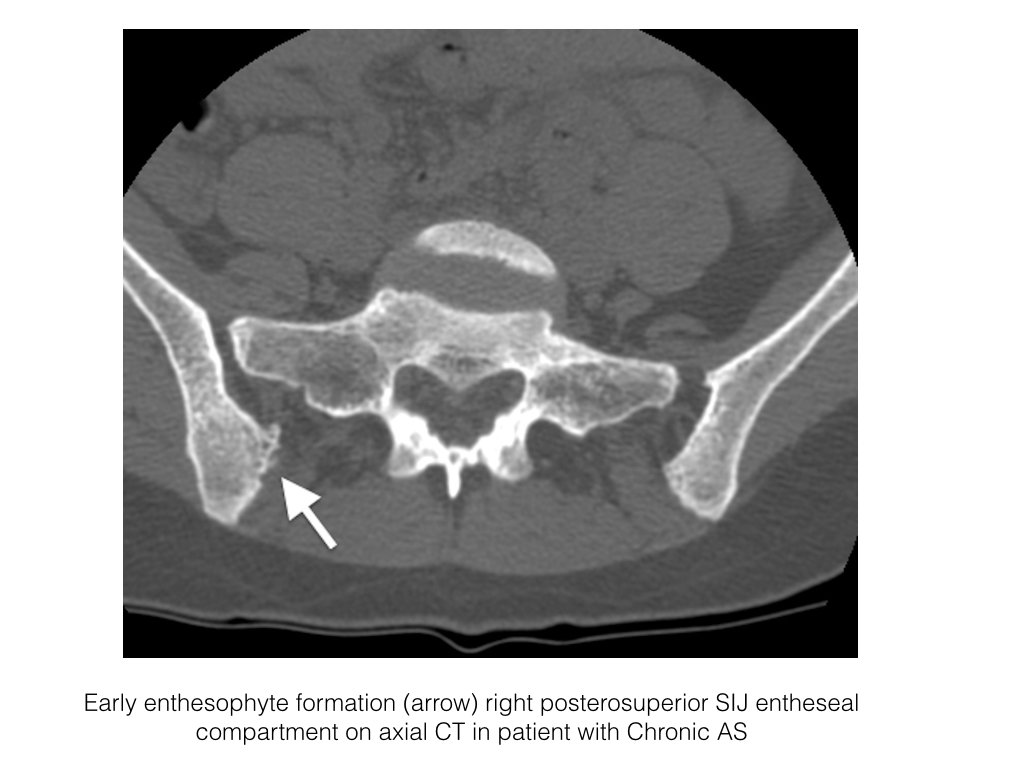
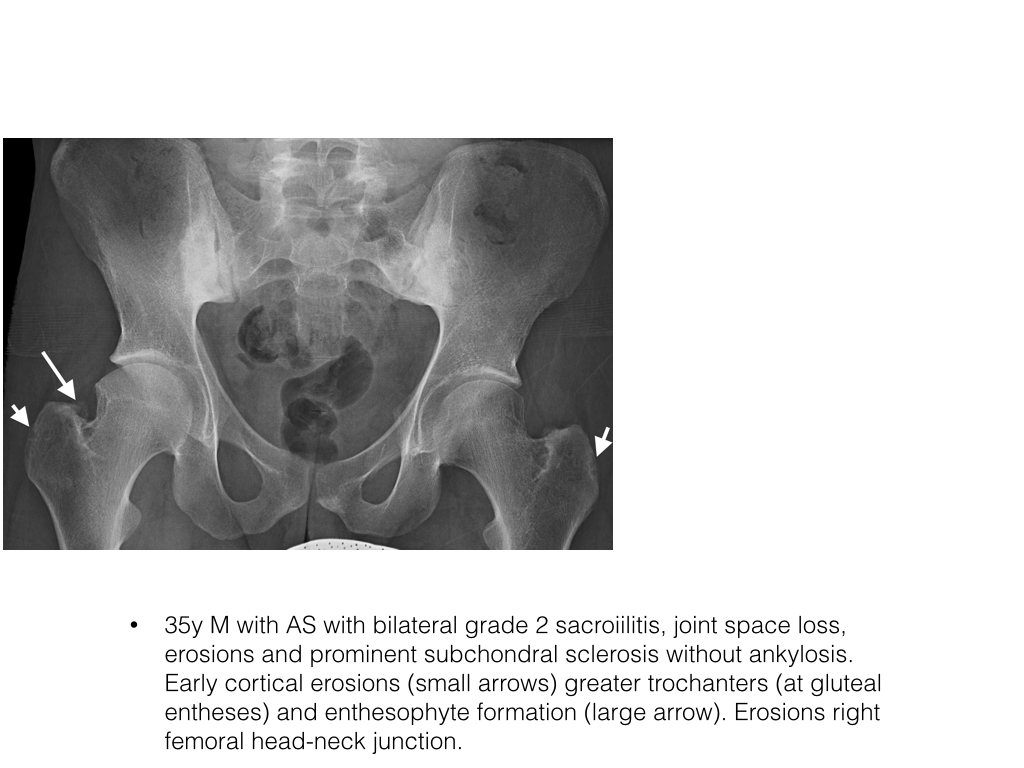
Enthesophytes
- An enthesophyte is new bone formation at an enthesis secondary to chronic stress or inflammation at the enthesis
- In axial disease it is usually best appreciated in the entheseal compartment of the SIJ.
- CT is the most sensitive. Small spikes of new bone can be seen at ligament insertion.
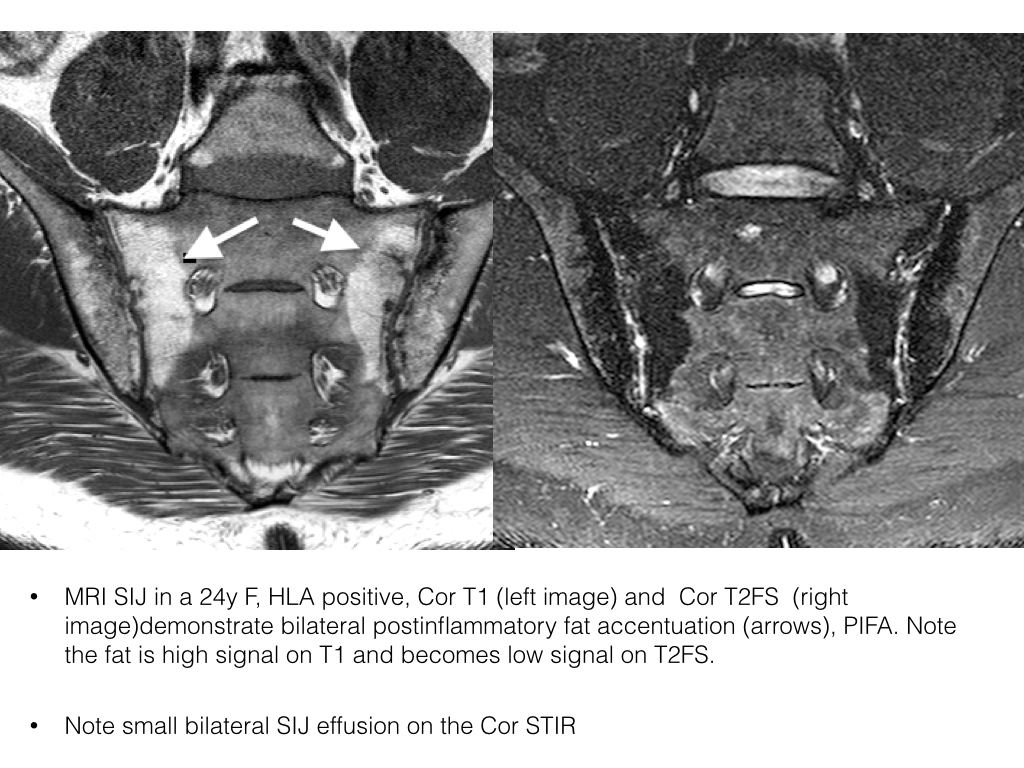
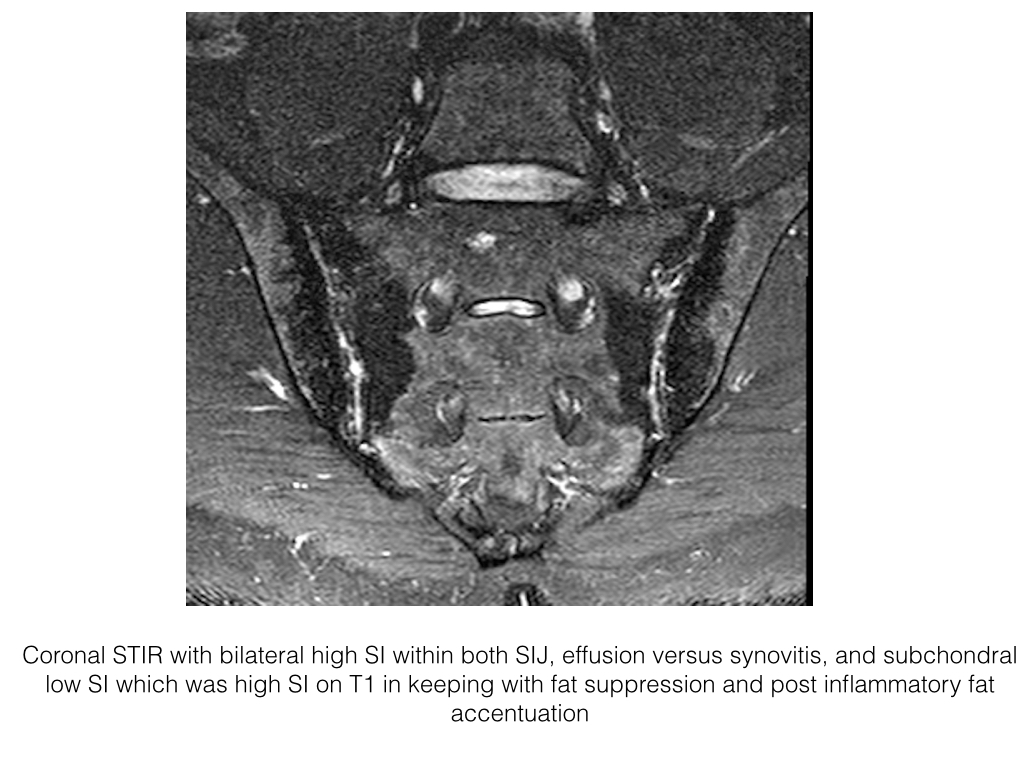
Joint Effusion
- An abnormal collection of fluid in a joint space
- Presentation in imaging includes intra-articular high signal intensity on STIR, low on T1, with no enhancement on contrast enhanced T1FS MRI.
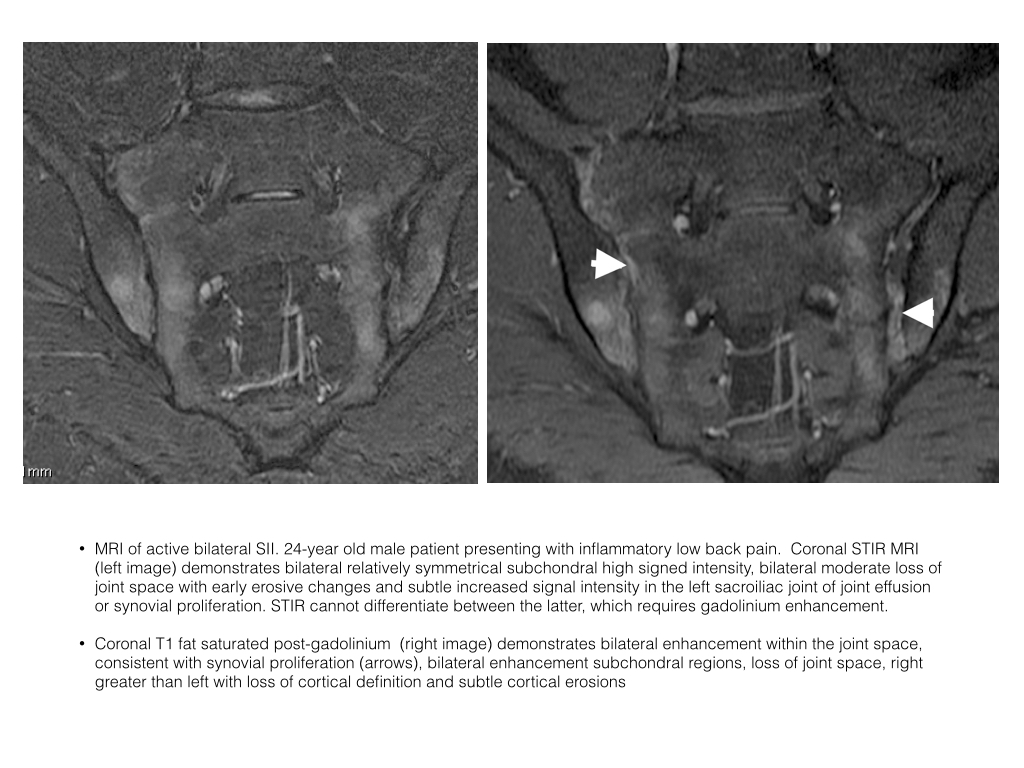
- Joint effusion and synovitis may appear similar on STIR, i.e. high signal intensity. Synovitis will enhance post gadolinium whereas an effusion will not.
- Capsular thickening and heterogenous signal intensity soft tissue within a joint suggests synovitis on a non-enhanced study
- Occurs at the sacroiliac joints and spinal facet joints
Synovitis
- Synovial tissue lines a synovial joint and is usually not visible on imaging.
- In synovitis the synovium proliferates, is inflamed and edematous and can appear like fluid on MRI i.e. low SI on T1 and high SI on T2FS and STIR.
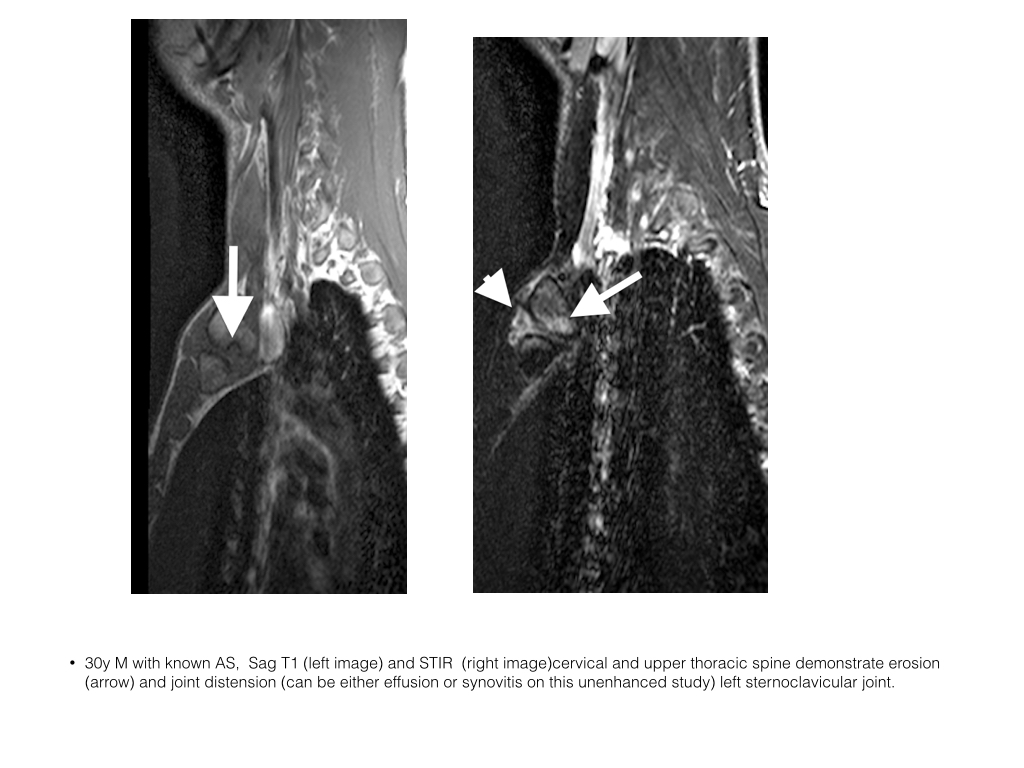
- Synovitis may occur in the sacroiliac joints, facet joints and sternoclavicular joints on spondylitis imaging
- With intravenous contrast synovium enhances whereas joint effusion does not
- Caveat: post contrast images should be fully acquired not longer than 10 minutes post injection as contrast may diffuse into a joint effusion and hence simulate a synovitis
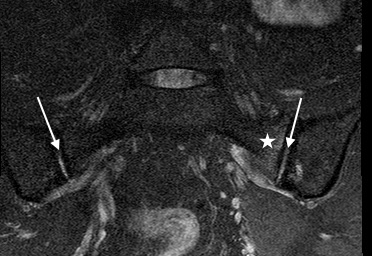
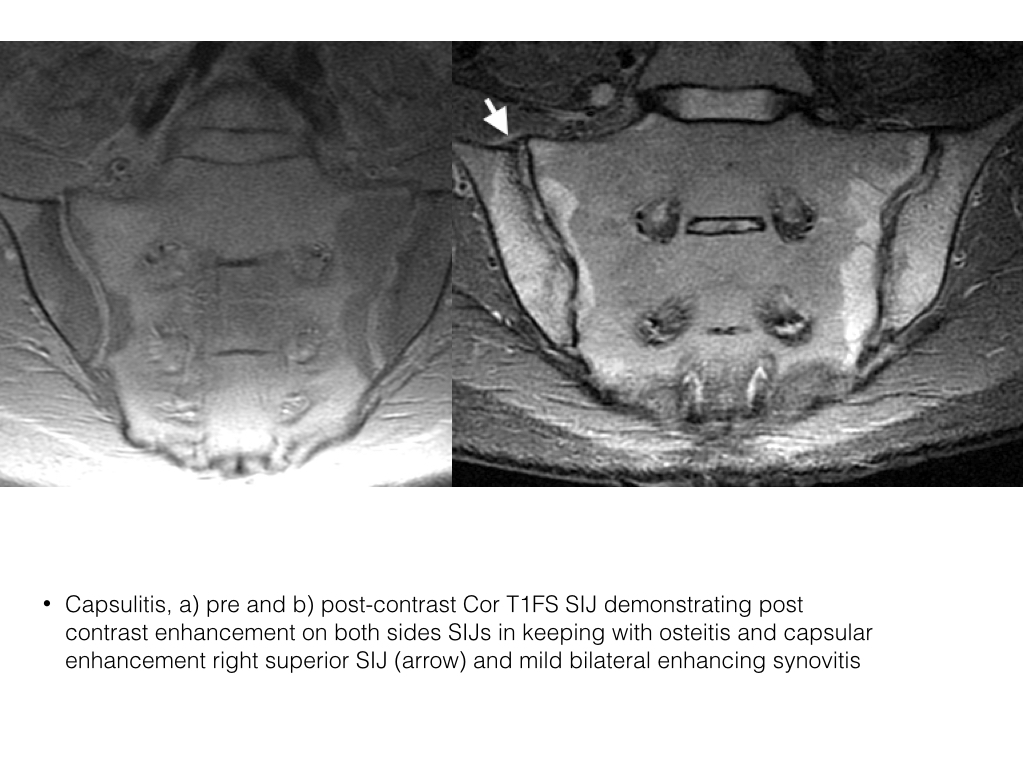
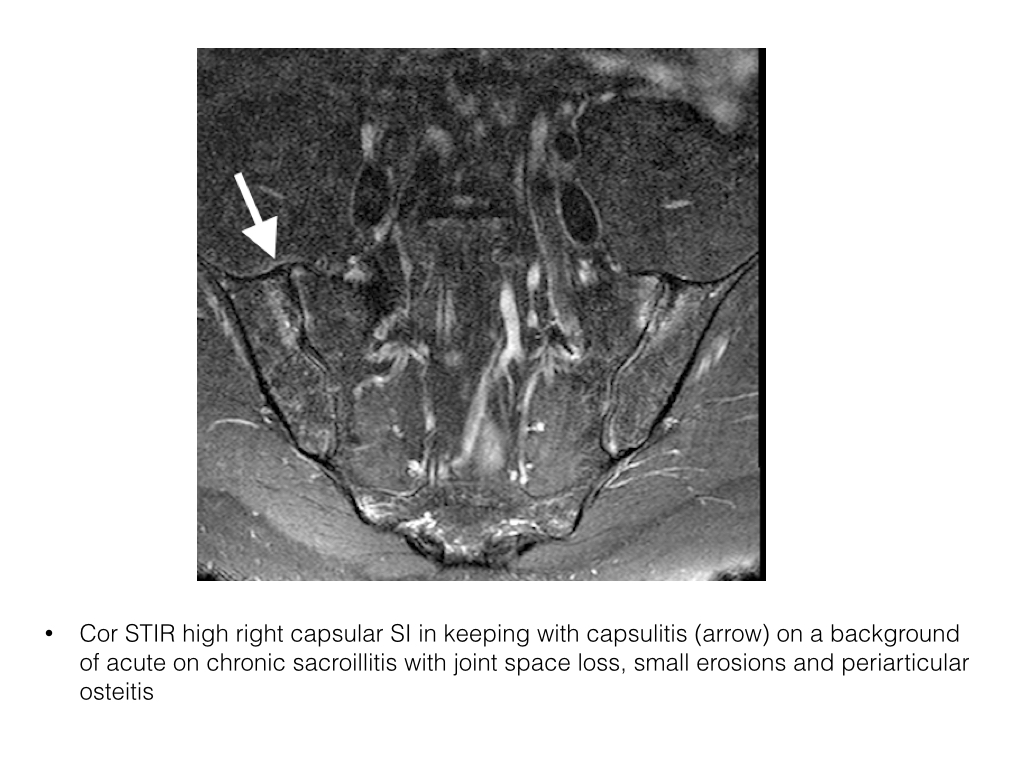
Capsulitis
- Refers to the inflammation of the capsule, a fibrous coating surrounding a joint or organ
- Capsulitis is the acute inflammation of the joint capsule and is only identifiable on MRI.
- Capsular high signal intensity is noted on STIR or contrast enhanced T1FS.
- May extend medially or laterally into the periosteum as an enthesitis
- Occurs in the sacroiliac joints (usually best seen along superior capsule) and the facet joints.
- Often seen in conjunction with other acute inflammatory changes
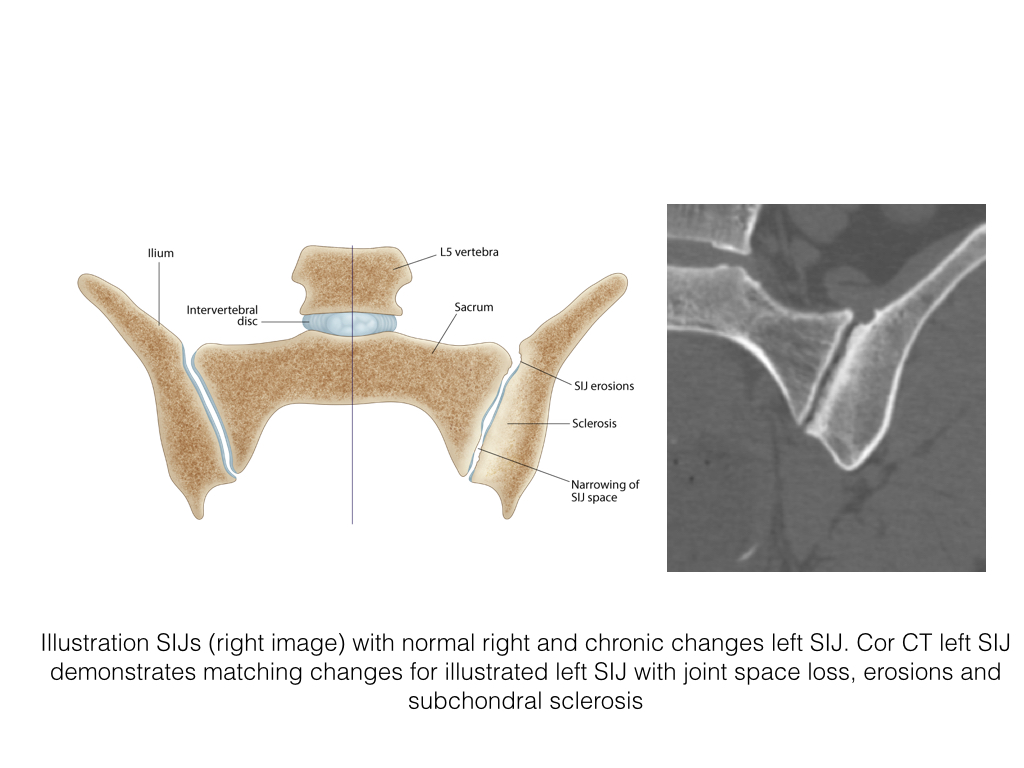
Erosions
- Erosions are non-anatomical (pathologic) focal cortical defects of bone secondary to an inflammatory process or local pressure effect and may be intra or extra-articular.
- Inflammatory processes include the inflammatory arthropathies such as AS, Rheumatoid arthritis, Psoriatic arthritis.
- Pressure erosions may occur in gout secondary to a gouty tophus. PVNS, pigmented villonodular synovitis, may cause intra-articular erosions from local mass effect.
- Erosions in axial SpA predominantly occur in the sacroiliac joints, the sternoclavicular joints and in the facet joints.
- CT is the gold imaging standard for erosions due to its high resolution and exquisite detail of bone architecture but is rarely required as MRI can also demonstrate acute inflammatory changes not visible on CT and incurs no radiation dose.
- In the SIJs coronal oblique T1FS images are the most sensitive for early erosions. Cartilage SI, high, is separable from fluid and synovitis and there is good discrimination between the cartilage and the low SI subchondral bone plate. However this sequence is not routinely used in clinical practice for the assessment of SpA, the commonly used sequences are Coronal oblique STIR and T1. Both demonstrate erosions. If there is an effusion present the STIR sequence is likely more sensitive due to contrast difference between the high SI fluid and low SI subchondral bone plate. The opposite is true if no fluid is present.
- Inactive erosions are low signal intensity on all imaging sequences.
- In active disease the erosion may be filled with fluid or synovitis, both high SI on T2, on its articular aspect and have reactive osteitis/edema within the adjacent subchondral marrow<./li>
- Cor T1FS is sensitive for erosions but will not demonstrate related osteitis or synovitis.
Post Inflammatory Fat Accentuation-SIJ
- PIFA, or fat deposition, is the presence of fat at sites of prior inflammation. In osteitis, i.e in active inflammation, the normal hemopoeitic cells in the marrow are displaced. When the inflammation resolves only marrow fat remains
- Since SIJ osteitis in SpA is periarticular so too is the fat deposition.
- PIFA is identified as periarticular high signal intensity on T1 and low signal intensity T1FS and STIR (both have fat suppression).
- Normal bone marrow signal intensity is assessed at the level of the sacral neural foramina and serves as a reference when assessing the periarticular region.
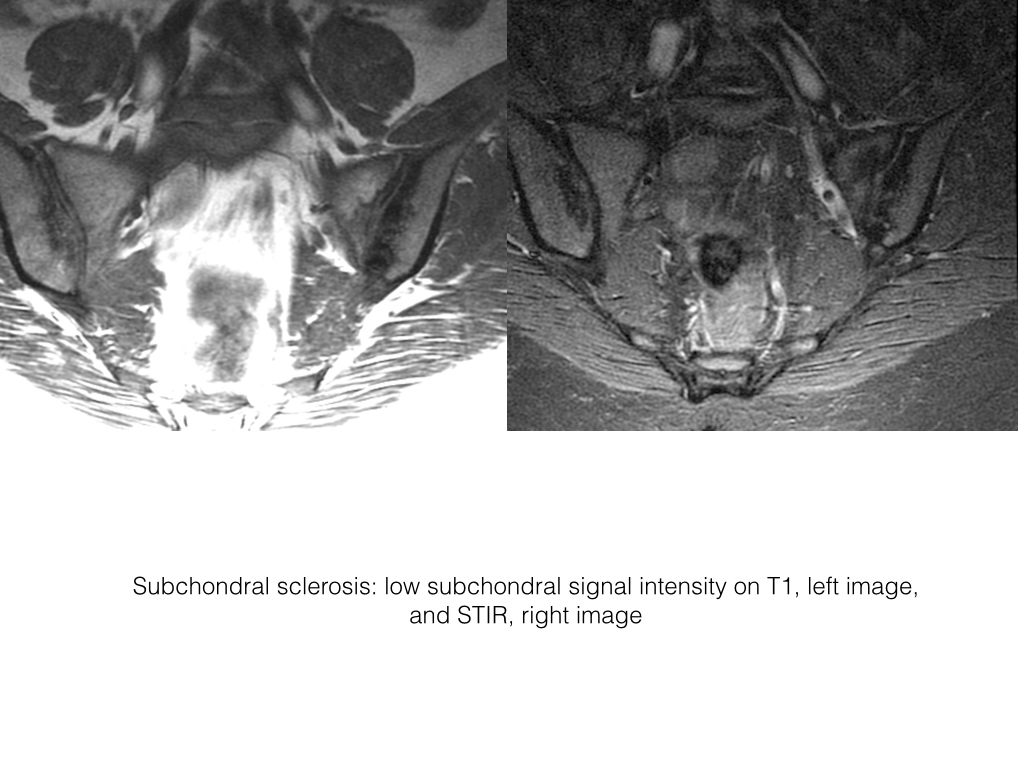
Subchondral Sclerosis
- With loss of the overlying articular cartilage the subchondral bone is exposed to increased stress across the joint. The bone responds with increasing trabecular collapse and flattening with subsequent increased attenuation bone on radiographs and CT.
- Subchondral sclerosis on MRI is low signal intensity on T1 and STIR. Most often seen at the SIJs but also evident at facet joints.
- Sclerosis is denser closer to the joint surface.
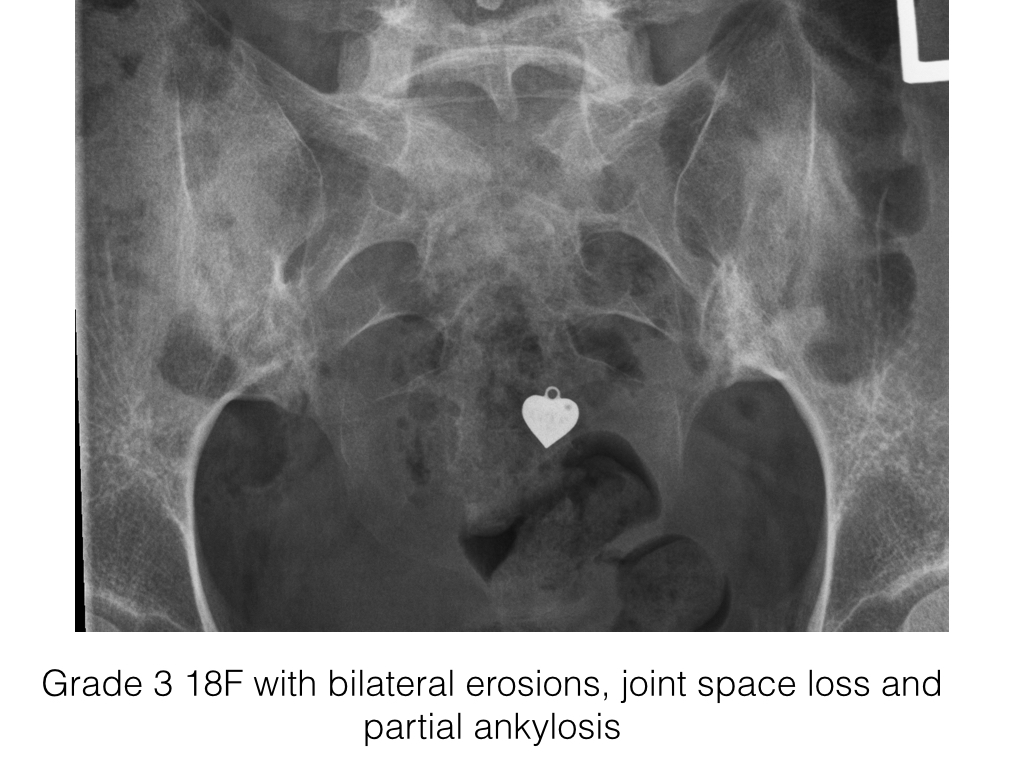
Ankylosis
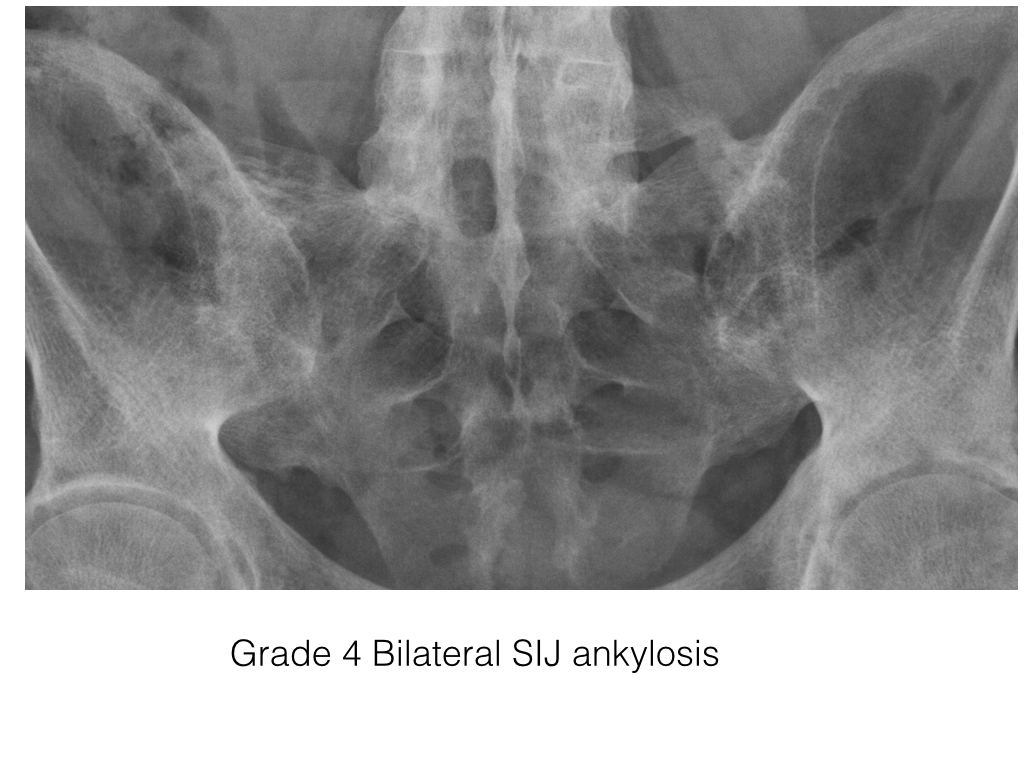
- On radiographs joint space is lost, the subchondral bone plate becomes indistinct and is eventually lost and bone trabecular can be seen transversing the previous joint space.
- CT is excellent in demonstrating bone detail and ankylosis.
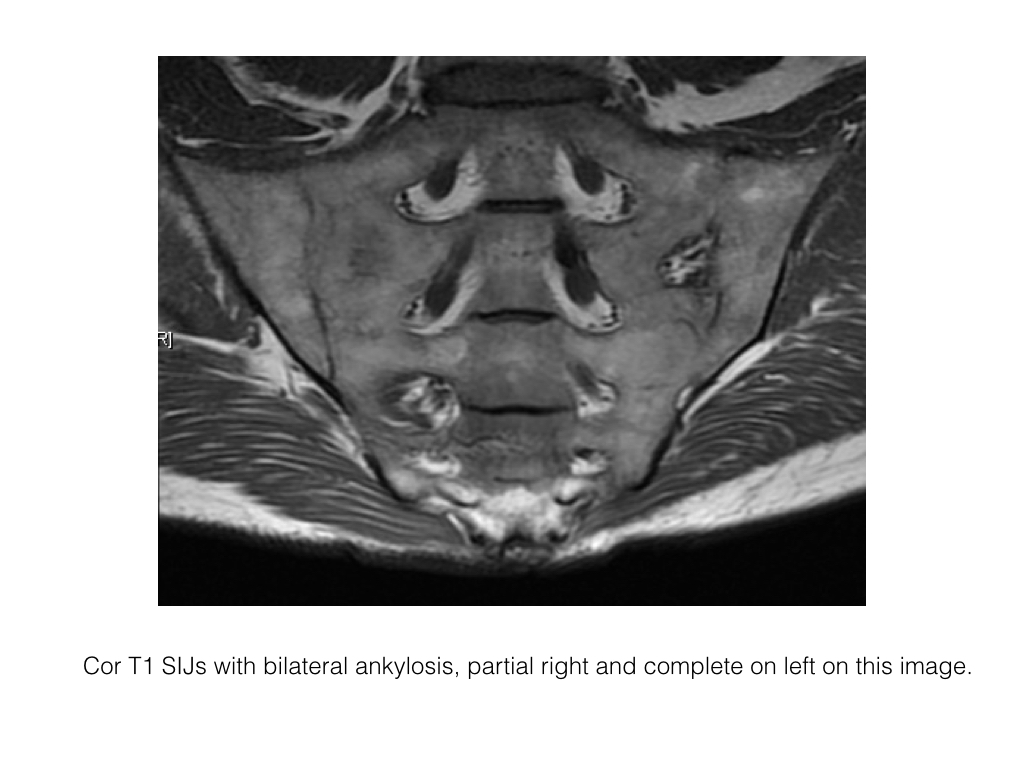
- MRI demonstrates continuation of bone marrow signal intensity across the previous joint space.
- Ankylosis occurs most commonly at the SIJs in SpA.
- In the spine the facet joints may become fused.
- In addition ligaments may ossify e.g. the supraspinous and interspinous ligaments (dagger sign on x-ray) and there may be apophyseal capsule ossification (trolley track sign)
 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline