Diagnostic & Classification Criteria
- A diagnostic criterion allows for the identification of a disease and allows the separation of those patients with the disease from the general population.
- Diagnostic criteria have a high sensitivity but lower specificity and are used in the diagnosis of the individual patient.
- Ideally diagnostic criteria would allow for the identification of patients throughout the spectrum of the disease, however in doing so will inadvertently include patients without the disease.
- Classification criteria allow for the systematic arrangement of similar entities on the basis of certain differing characteristics creating a homogenous group with a high specificity but low sensitivity for the disease.
- Classification criteria are often used in clinical research in patients with a known disease however have a low sensitivity for early disease and do not automatically apply to the general population.
Diagnosis SpA?
- In many rheumatological diseases there are well-established classification criteria but less well-formed diagnostic criteria. This holds true for SpA.
- Criteria applied to date for axial spondyloarthropathy are classification criteria and include the following:
- Modified New York
- Amor
- ESSG (European Spondyloarthropathy Study Group)
- ASAS (Assessment of SpondyloArthritis International Society)
The current gold standard for diagnosis of SpA is the expert opinion of a rheumatologist of the clinical and imaging findings.
- The modified New York Criteria is helpful in the radiographic assessment of the sacroiliac joints and diagnosis chronic sacroiliitis.
- The ASAS criteria include MRI, the gold standard in imaging SpA, and is not present in the other criteria.
- We will review both criteria.
Modified New York Grading Criteria for Ankylosing Spondylitis
- Clinical Criteria
- Low back pain present for at least 3 months not relieved by rest and improves with exercise
- Limited lumbar spine motion in sagittal and frontal planes
- Limited chest expansion*
- Radiological Criteria
- Sacroiliitis: Grade 2 bilaterally or unilateral grade 3-4
- Ankylosing Spondylitis if radiological criteria plus one clinical criteria
*Relative to normal values for age and sex.
Modified New York Radiographic Grading
Grade |
Imaging Findings |
| Grade 0 | Normal |
| Grade 1 | Suspicious Change |
| Grade 2 | Minimal Abnormality-small localised areas with erosion or sclerosis without alteration in joint width |
| Grade 3 | Definite Abnormality- moderate or advanced disease including partial ankylosis |
| Grade 4 | Severe abnormality- total ankylosis |
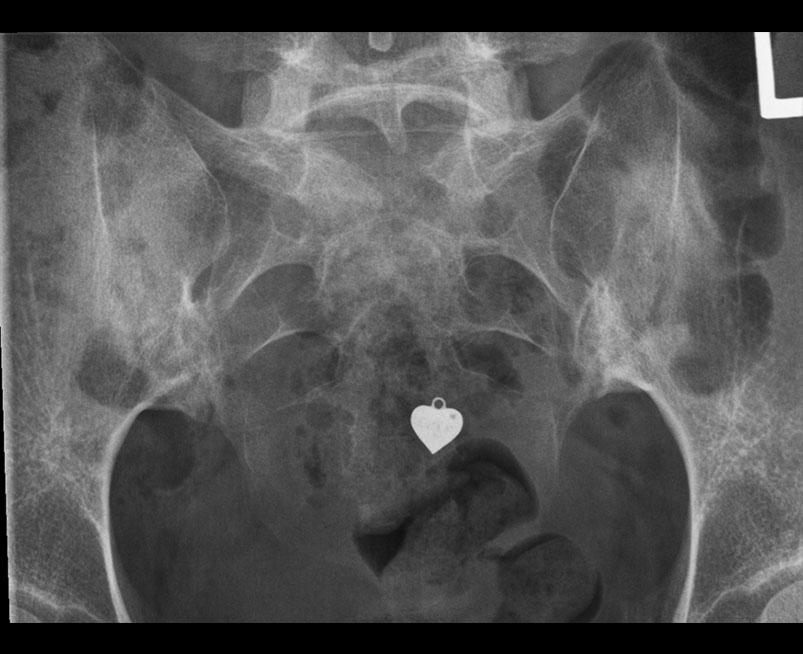
New York Modified Grading Criteria
- Plain radiography has and continues to play an important role in the investigation of SII and is an integral part in the diagnosis of AS.
- The anatomy of the sacroiliac joint, due to its oblique nature and overlap of the sacral and iliac components, has led to significant inter- and intra- observer variations particularly in the interpretation of early SII.
- Differentiation from normal patients is particularly problematic in women and in older age groups where early degenerative changes may simulate early SII.
- Plain radiographs of the sacroiliac joint can be performed and include dedicated AP and bilateral oblique views.
- However AP radiograph of the lumbar spine often clearly demonstrates the sacroiliac joints and if fully included has been shown to be as sensitive as a dedicated AP of the SIJ.
- Some centres advocate a baseline AP pelvis. This allows for assessment of the sacroiliac joints and the hip joints, the latter is involved in up to 25% of patients with SpA.
- Plain radiography should be performed as the initial imaging modality.
New York Modified Grading Criteria
- Radiographic changes include:
- periarticular osteopenia
- erosions
- initial joint space widening progressing to narrowing joint space in later disease
- subchondral sclerosis
- bony ankylosis
- The modified New York criteria includes radiographs as a key component in the diagnosis of AS.
- Grade 2 -4 bilateral disease or unilateral Grade 3-4 disease with one clinical criterion was required for the diagnosis. Involvement of the spine was not included in this criteria set.
ASAS Criteria for Axial Spondyloarthropathy
- In patients with >= 3 months back pain with age of onset < 45yrs
- Sacroiliitis on Imaging* plus >/=1SpA clinical feature
or
HLA B27 positive plus>= 2other SpA clinical features
Clinical Features:
- Inflammatory back pain (ASAS criteria)
- Dactylitis° (sausage digit)
- Psoriasis°
- Positive family history of SpA (First or second degree relative with any of the following: AS, Psoriasis, Uveitis, Reactive Arthritis, IBD
- Good response to NSAIDs (24-48 hrs post full dose back pain absent or significantly improved)
- Enthesitis (heel)
- Arthritis°
- Crohn’s/Colitis disease °
- Elevated CRP in presence of back pain without alternate cause
- HLAB27 positive
- Uveitis°
ASAS Inflammatory Back Pain Criteria
- Insidious onset
- Age of Onset less than 40 years
- Improvement with exercise
- Pain at night, improved on getting up
- No improvement with rest
ASAS Criteria
- However it has set significant internal limitations. MRI findings are based solely on the presence of active sacroiliitis.
- Active sacroiliitis by ASAS definition has been documented in 7% of normal control subjects and 23% patients with non-specific back pain.
- The ASAS criteria exclude all other MRI changes related to acute and chronic disease of the sacroiliac joints and the spine.
- It does however include the New York radiographic changes of unilateral grade 3-4 or bilateral grade 2 disease.
- As such the current imaging component of the ASAS criteria are limited when assessing the individual patient.
- New EULAR recommendations, detailed in the following pages, takes the imaging diagnosis of SpA forward in recognizing the important of the presence of chronic/structural changes of sacroiliitis which we use in everyday clinical practice.
- With the increasing recognition of spondyloarthropathy in the general population there has been a significant increase in the number of requested imaging studies, ten-fold at our centre in the last decade. With this increased referral there has also been an increase in the number of patients demonstrating subtle non-specific findings, including edema, which may represent early sacroiliitis or be related to prior trauma (including pregnancy) and degenerative disease.
- When the clinical arm is non-diagnostic we often advise follow-up imaging in these cases in 6 months to 1 year but treat each case individually.
- Close clinical interaction between the Rheumatology and Diagnostic Imaging services are essential for optimal patient care. We emphasize again that the gold standard for the diagnosis of SpA
- Please see new proposed MRI Axial SpA Image Categorization section
Eular Recommedations
- EULAR recommendations for the use of imaging in the diagnosis and management of spondyloarthritis in clinical practice, Mandi et al,Ann Rheum Dis 2015;74:1327-1339
- A taskforce comprised of an expert group of 21 rheumatologists, radiologists and methodologists from 11 countries developed evidence-based recommendations on the use of imaging in the clinical management of both axial and peripheral spondyloarthritis (SpA).
- Ten recommendations were produced using research-based evidence and expert opinion encompassing the role of imaging in making a diagnosis of axial SpA or peripheral SpA is the expert opinion of a rheumatologist of the clinical and imaging findings. Monitoring inflammation and damage, predicting outcome, response to treatment, and detecting spinal fractures and osteoporosis. those related to axial spondyloarthropathy are presented here.
Diagnosis
- A. In general, conventional radiography of the SI joints is recommended as the first imaging method to diagnose sacroiliitis (variable sen/spec 84/75).
- In certain cases, such as young patients and those with short symptom duration, MRI of the SI joints is an alternative first imaging method.
- B. If the diagnosis of axial SpA cannot be established based on clinical features and conventional radiography, and axial SpA is still suspected, MRI of the SI joints is recommended. On MRI, both active inflammatory lesions (primarily bone marrow edema) and structural lesions (such as bone erosion, new bone formation, sclerosis and fat infiltration) should be considered. MRI of the spine is not generally recommended to diagnose axial SpA.
- C. Imaging modalities, other than conventional radiography and MRI are generally not recommended in the diagnosis of axial SpA*.
- SOR 9.5 (9.2–9.8), LOE Level III
MRI increased sen/spec when erosions included with bone marrow edema
Monitoring Activity
- MRI of the SI joints and/or the spine may be used to assess and monitor disease activity in axial SpA, providing additional information on top of clinical and biochemical assessments.
- The decision on when to repeat MRI depends on the clinical circumstances. In general, STIR sequences are sufficient to detect inflammation and the use of contrast medium is not needed.
- SOR 9.2 (8.8–9.6), LOE Level 1B
Monitoring Structural Changes
- Conventional radiography of the SI joints and/or spine may be used for long-term monitoring of structural damage, particularly new bone formation, in axial SpA.
- If performed, it should not be repeated more frequently than every second year. MRI may provide additional information (limited studies to determine exact role at this time).
- SOR 9.3 (8.8–9.8), LOE Ib
Predicting outcome/severity
- In patients with ankylosing spondylitis (not non-radiographic axial SpA), initial conventional radiography of the lumbar and cervical spine is recommended to detect syndesmophytes, which are predictive of development of new syndesmophytes.
- MRI (vertebral corner inflammatory or fatty lesions) may also be used to predict development of new radiographic syndesmophytes.
- SOR 9.0 (8.5–9.5), LOE Ib
Predicting Treatment Effect
- Extensive MRI inflammatory activity (bone marrow edema), particularly in the spine in patients with ankylosing spondylitis, might be used as a predictor of good clinical response to anti-TNF-alpha treatment in axial SpA.
- Thus, MRI might aid in the decision of initiating anti-TNF-alpha therapy, in addition to clinical examination and CRP.
- SOR 8.9 (8.3–9.5), LOE Ib
Spinal fracture
- When spinal fracture in axial SpA is suspected, conventional radiography is the recommended initial imaging method. If conventional radiography is negative, CT should be performed. MRI is an additional imaging method to CT, which can also provide information on soft tissue lesions.
- SOR 9.3 (8.9–9.7), LOE IV
Osteoporosis
- In patients with axial SpA without syndesmophytes in the lumbar spine on conventional radiography, osteoporosis should be assessed by hip DXA and AP-spine DXA.
- In patients with syndesmophytes in the lumbar spine on conventional radiography, osteoporosis should be assessed by hip DXA, supplemented by either spine DXA in lateral projection or possibly QCT of the spine.
- SOR 9.4 (9.0–9.8), LOE III
 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline
 info_outline
info_outline